Nursing literature abounds with descriptive and predictive studies of structural empowerment and its relationship to nurses’ trust, commitment, control over practice, intent to stay, productivity, job satisfaction, engagement, and quality of care. This article explores the links between the Magnet® Model and structural empowerment in the workplace
Structural empowerment is one of the five components of the Magnet Model. The others are transformational leadership; exemplary professional practice; new knowledge, innovations, and improvements; and empirical outcomes.
Within the context of the Magnet Model, structural empowerment encompasses organizational structure, personnel policies and programs, professional development, community outreach, and promotion of a positive nursing image. How do these elements reflect structural empowerment? Here are a few examples:
- Establishing a “just culture” supports professional accountability and error reporting in an effort to improve patient safety rather than punish or ostracize people for their mistakes.
- Creation of a peer-review council allows those “in the know” to conduct performance evaluation, not those far removed from the work.
- The shared governance philosophy plays out in decision-making policies.
Through transformational leadership, organizational structure, transparency, congruence of mission with day-to-day operations, and the work environment, a healthcare organization is either “magnetized” or not. Today’s healthcare leaders are expected not just to empower staff, solve problems, and adapt to change. To truly embrace healthcare reform in creative ways, they also must foster a certain degree of controlled destabilization that births new ideas and innovations. People (not only staff but also patients and families) should feel comfortable asking questions.
A structurally empowered nurse is best equipped to protect patients’ rights. A Magnet organization focuses not just on improving its own performance but also on contributing new knowledge to the science of nursing. It’s expected to use the latest research-based evidence in all of its practices.
Exemplary professional practice in a Magnet organization transcends the organization itself and extends to the practice of nursing as a whole. One way to transcend the organization is through community outreach. A strong professional nursing practice in a Magnet organization should be palpable in the community. An empowered nurse who’s involved in committees and task forces that influence change in the hospital also may serve on community boards. In this way, she or he leaves a nursing imprint on healthcare policies outside the hospital. When hospital leaders support this nurse’s community involvement, they’re demonstrating structural empowerment.
Even a nurse who works in one of the most restricted hospital settings—the perioperative area—can project a positive image of nursing in the community. For instance, she may volunteer to provide surgical care for people in need locally, regionally, nationally, or even globally. Or she may serve as the hospital’s laser safety officer, seeking input from nurses and other staff who work with surgical lasers and interfacing with laser industry representatives while keeping patients’ best interests in mind. In this role, she’s demonstrating the value of patient advocacy to technical, research and development, and marketing professionals. Thus, she promotes an understanding of what nurses do first and foremost—preserve patient safety.
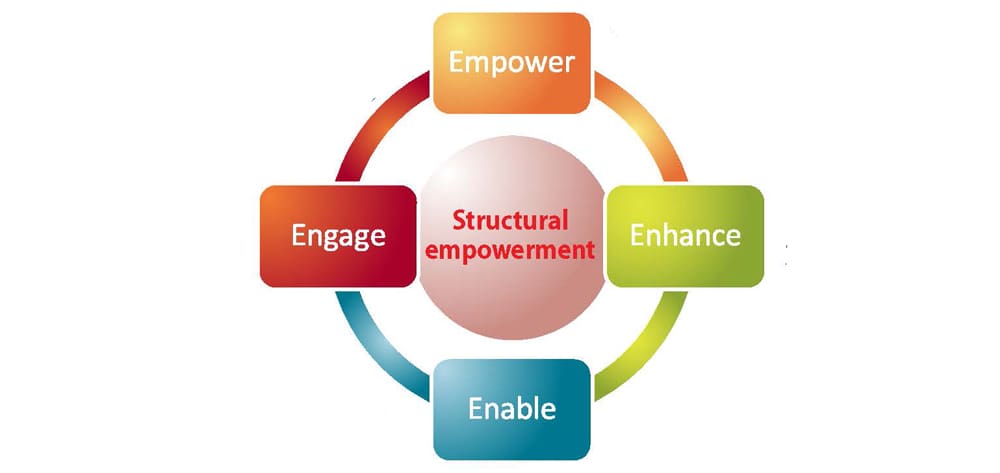
Factors that promote structural empowerment
First described in 1977, the theory of structural empowerment posits that certain factors in a work environment can enable or block employees’ ability to accomplish their work in meaningful ways. The four empowerment structures are:
- access to resources needed for one’s work
- access to information needed to get one’s job done as well as knowledge and understanding of the organization
- support for one’s responsibilities and job performance
- opportunity for professional growth and development.
Having formal and informal power enhances these factors.
How does your workplace stack up?
Consider whether the empowerment structures described above are present in your workplace.
- Does your environment help you accomplish your work in meaningful ways? Do you have access to the resources needed for your work? Do you have the time and appropriate resources with which to accomplish your work?
- Do you have access to the information you need to get the job done? Do you know the values and goals of your hospital’s leaders? Are you aware of its financial status? Do you know the future direction leaders want to take the hospital?
- Do you feel your manager supports your responsibilities and job performance? Does your manager provide specific information about tasks you do well? Does he or she give you tangible recommendations on how you can improve? Do you believe your work is valued? What about rewards for contributing innovative ideas and showing flexibility in your job?
- Is your work visible within the organization as a whole? Do you work collaboratively with physicians and other healthcare team members? Do they work collaboratively with you? Do peers and managers seek your help with problems?
- Does your employer give you the opportunity for professional growth and development? Is your work challenging? Does it offer a chance to learn new skills and gain new knowledge? Do you have opportunities to use all of your skills and knowledge? Do you believe your workplace is an empowering environment overall? (Note: These questions come from the Conditions of Work Effectiveness Questionnaire, which measures structural empowerment within the work setting.)
If you answered no to some of these questions, it doesn’t necessarily mean you work in a negative organization—just that there’s room for growth and a need for change. You may be able to change some things yourself. For example, perhaps access to information is present but you’re not taking advantage of it. Maybe your supervisor has given you recommendations but you haven’t heeded them. On the other hand, perhaps the leadership mindset at your organization needs to be transformed. Being candid with your employer about your perceptions may lead to strategies to improve the environment.
Cultivating an exceptional work environment doesn’t happen overnight. To use a term that occurs throughout Magnet literature, this truly is a journey. Be patient, be engaged, and get involved in the improvement process to maximize structural empowerment in your workplace.
Selected references
Kanter RM. Men and Women of the Corporation. 2nd ed. New York, NY: BasicBooks; 1993.
Magnet Recognition Program® Model. American Nurses Credentialing Center. (2014). www.nursecredentialing.org/magnet/programoverview/new-magnet-model. Accessed July 2, 2014.
Moore SC, Hutchison SA. Developing leaders at every level: accountability and empowerment actualized through shared governance. J Nurs Adm. 2007;37(12):564-8.
Moore SC, Wells NJ. Staff nurses lead the way for improvement to shared governance structure. J Nurs Adm. 2010;40(11):477-82.
Schroeter K. Structural empowerment: the Magnet model applied to perioperative nursing. AORN J. 2010;92(2):220-3.
Spence Laschinger, HK. CWEQ: Conditions of work effectiveness questionnaire I and II. (n.d.). http://publish.uwo.ca/~hkl/tools/cweq/index.html. Accessed July 2, 2014.
Spence Laschinger HK, Wilk P, Cho J, Greco P. Empowerment, engagement and perceived effectiveness in nursing work environments: does experience matter? J Nurs Manag. 2009;17(5):636-46.
Tinkham MR. Pursuing Magnet designation: the role of structural empowerment. AORN J. 2013;97(2): 253-6.
Walker KN, Duff J, Di Staso R, et al. Perioperative nursing shines! Magnet designation reflected in staff engagement, empowerment and excellence. Acorn: J Periop Nurs Austr. 2011;24(3):34-42.
Shelley Moore is an assistant professor at Middle Tennessee State University School of Nursing in Murfreesboro.