Martin Pace, a 65-year-old man, is admitted with an inferior wall ST-segment elevation myocardial infarction and receives a permanent pacemaker for sick sinus syndrome. When he returns to the progressive care unit, he’s awake, alert, and cooperative. His blood pressure (BP) is 125/70 mm Hg, respiratory rate (RR) 14 breaths/minute, oxygen saturation (O2 sat) 98% on room air, and he has a paced rhythm of 60 beats/minute (bpm). The postprocedure chest X-ray shows the pacing wires are in good position. Mr. Pace says he’s comfortable with no pain.
 Key takeways
Key takeways
– Acute cardiac tamponade occurs quickly and can be caused by trauma, aortic dissection, ventricular rupture, or as a complication of any invasive procedure that manipulates great vessels.
– Early signs and symptoms include dramatic changes in physical assessment, evidence of right-sided heart failure, narrowing of pulse pressure, pulsus paradoxus, shortness of breath, tachypnea, and decreased urine output.
– Prompt treatment requires quick assessment and use of rapid response teams.
Assessment
Mr. Pace’s nurse, John, notices on telemetry that his HR has increased along with a change to sinus rhythm, rate 88 bpm. Mr. Pace is short of breath with an RR of 22 breaths/minute, and his BP is 120/78 mm Hg.
John elevates the head of Mr. Pace’s bed and performs a quick assessment, which reveals a neurologically awake and alert patient who is moving all extremities equally, cool skin with equal pulses, BP 105/80 mm Hg, clear lungs with O2 sat 96% on room air, and RR 26 breaths/minute. John also notes bilateral jugular vein distention (JVD). Mr. Pace says he’s not in pain.
John calls for a rapid response team (RRT) consultation for cardiac decompensation after pacemaker insertion.
Rapid response
 When the RRT arrives, John has already placed Mr. Pace on oxygen at 2 L/min by nasal cannula, with bedside continuous electrocardiogram (ECG) monitoring, continuous noninvasive BP monitoring, and an 18-G I.V. with normal saline infusing. John also called for a 12-lead ECG, which is being completed at the bedside.
When the RRT arrives, John has already placed Mr. Pace on oxygen at 2 L/min by nasal cannula, with bedside continuous electrocardiogram (ECG) monitoring, continuous noninvasive BP monitoring, and an 18-G I.V. with normal saline infusing. John also called for a 12-lead ECG, which is being completed at the bedside.
The RRT notes that Mr. Pace is in a progressive shock state. A normal saline bolus of 500 mL is given, and portable chest X-ray and multiple serum labs with a serum lactate are ordered. With fluid administration, Mr. Pace’s BP begins to improve.
The 12-lead ECG shows sinus tachycardia with no ischemia or infarction. Mr. Pace’s chest X-ray reveals a widened mediastinum with a small right pleural effusion. Hemoglobin and hematocrit are slightly lower than previous readings, coagulation studies are normal, and serum lactate is 3.8 mmol/L (normal is below 1.5 mmol/L).
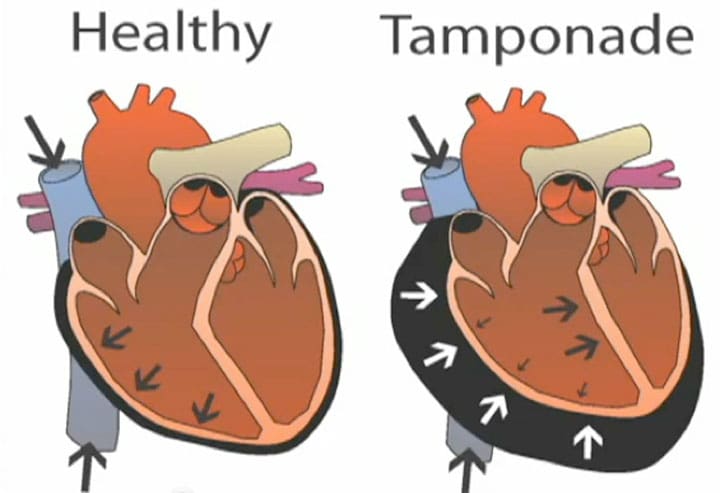
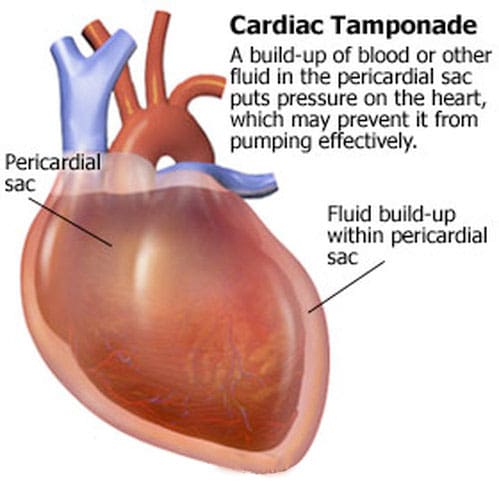
An echocardiogram shows moderate pericardial effusion with right-sided compromise and low left ventricular output as a result of low filling volumes of the left ventricle. A diagnosis of cardiac tamponade is made.
The patient is taken to the cardiac catheterization laboratory, where, under fluoroscopy, the tamponade is tapped for 350 mL of bloody effusion. After the procedure, Mr. Pace’s vital signs are normal, and his serum lactate falls to 1.8 mmol/L.
Outcome
Mr. Pace returns to the telemetry unit, where John continues to monitor him, obtaining vital signs every 30 minutes for 2 hours, then every hour. A repeat ECG shows normal left ventricular filling and function. Discharge planning includes a return office visit with a repeat ECG at 1 week.
A dangerous development
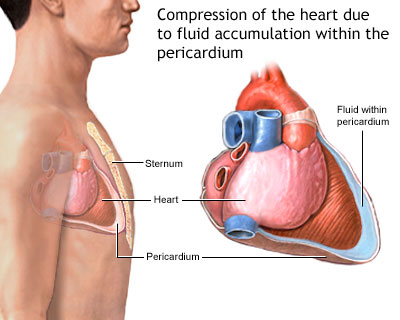
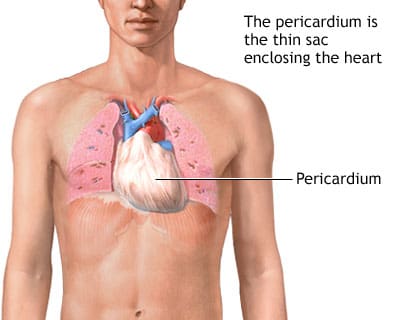
Acute cardiac tamponade occurs quickly and can be caused by trauma, aortic dissection, ventricular rupture, or as a complication of any invasive procedure where the great vessels are manipulated (such as a permanent pacemaker or central line insertion). Other causes include a slow right ventricular leak or slowly occurring fluid accumulation that leads to acute signs and symptoms.
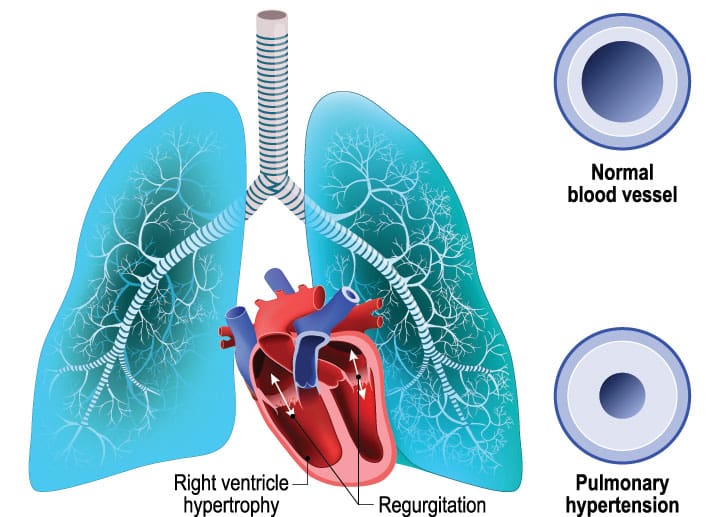
Early signs and symptoms include dramatic changes in physical assessment, evidence of right-sided heart failure (tachycardia, increased JVD, clear lungs, signs of poor perfusion), narrowing of the pulse pressure (normal is 35 to 45 mm Hg) causing a drop in systolic blood pressure, pulsus paradoxus (more than 10 mm Hg drop in systolic blood pressure with inspiration), shortness of breath, tachypnea, and decreased urine output. Beck triad refers to three classic signs indicating cardiac tamponade—JVD, hypotension, and muffled heart sounds on auscultation.
Although there aren’t any specific laboratory tests for cardiac tamponade, serum lactate may be elevated because of reduced peripheral perfusion as a result of decreased cardiac output. Differential diagnoses include myocardial infarction, pulmonary embolism, tension pneumothorax, and constrictive pericarditis.
Thanks to John’s quick assessment and action, Mr. Pace’s cardiac tamponade was identified and treated quickly.
Mary Ann House-Fancher is an acute care nurse practitioner in the department of critical care medicine at the University of Florida, Shands Hospital in Gainesville.
Selected references
Adler Y, Charron P, Imazio M, et al; European Society of Cardiology (ESC). 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2015;36(42):2921-64.
National Institute for Health and Care Excellence (NICE). Clinical guideline 174: Intravenous fluid therapy in adults in hospital: Algorithm for assessment and fluid resuscitation. Updated May 2017.
Spodick DH. Acute cardiac tamponade. N Engl J Med. 2003;349(7):684-90.
Wilson JG, Epstein SM, Wang R, Kanzaria HK. Cardiac tamponade. West J Emerg Med. 2013;14(2):152.
Yarlagadda C. Cardiac tamponade clinical presentation. Medscape. Updated November 20, 2016.















1 Comment.
Hello, I wonder if we could please use the image of the normal heart versus the tamponading heart for educational purposes on a not for profit trauma course- Western Trauma Course.
Kind Regards
Georgina