Pressure injury prevention requires an effective and sustainable program
By Melissa A. Fitzpatrick, MSN, RN, FAAN
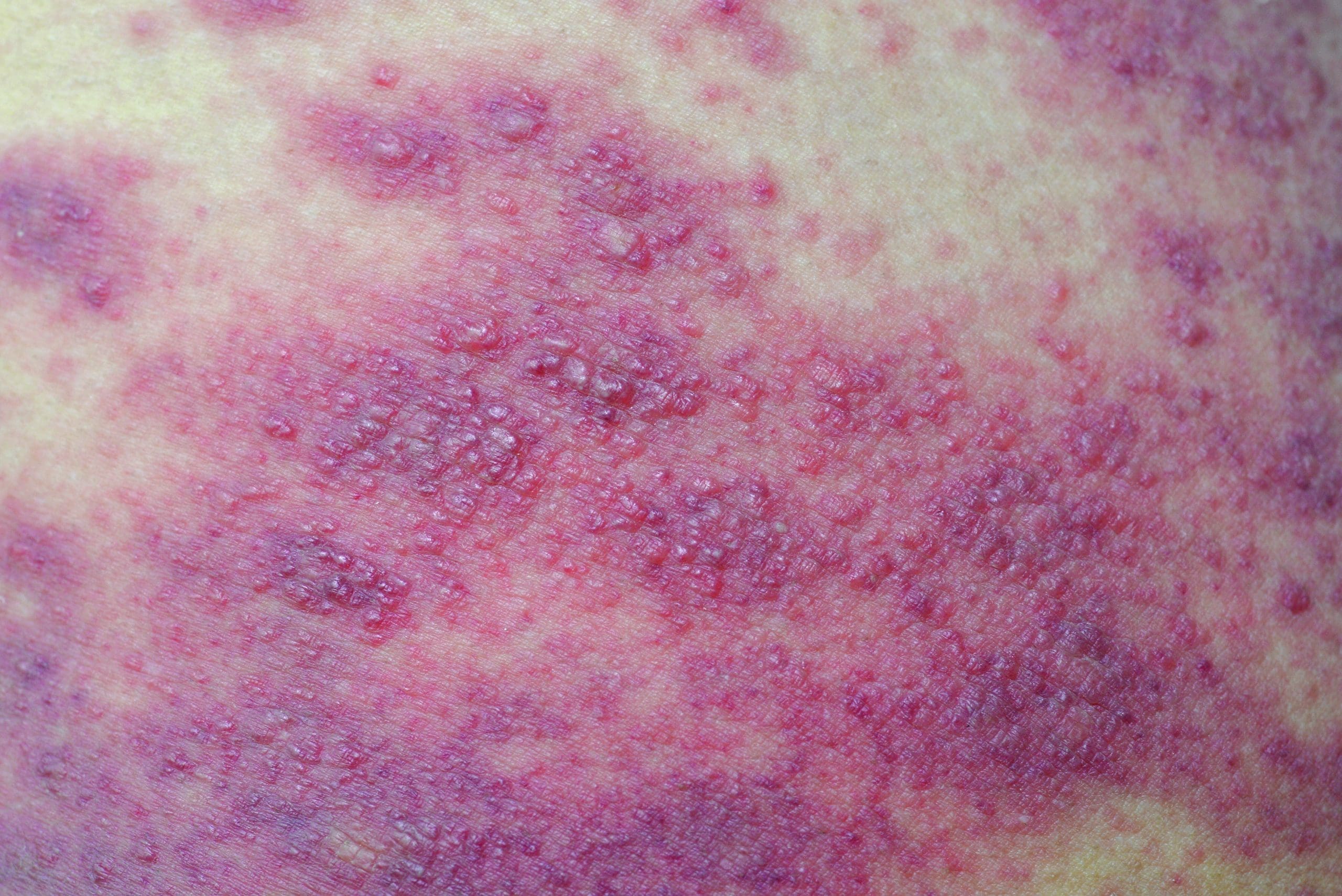
Pressure injuries (PIs) have presented a significant risk to patients and a clinical challenge to nurses and other clinicians since before nursing became a profession. The skin is the largest organ of the body and although it doesn’t get the same attention as the heart, brain, liver, and lungs, it can be the most serious threat to a patient’s survival or at the very least, to his or her comfort and well-being. How often does a critical- care team work diligently to revive a patient in cardiogenic shock only to have him succumb to an infected PI? What about the perioperative team that toils over the neurosurgical patient to successfully restore function only to have her succumb postoperatively from the sequelae of a deep-tissue injury?
 We know from the National Pressure Ulcer Advisory Panel that not all PIs areavoidable, but we also know that most are when excellent assessment, physical care, multidisciplinary teamwork, and technology are used to ensure adequate perfusion.
We know from the National Pressure Ulcer Advisory Panel that not all PIs areavoidable, but we also know that most are when excellent assessment, physical care, multidisciplinary teamwork, and technology are used to ensure adequate perfusion.
Never have our patients needed these caregiving elements more than today. With patient acuity, age, and comorbidities rising, risk for all so-called “never events” like PI has escalated as well. Those risk factors follow patients across the acute care continuum, so an effective PI-prevention program must include many care environments—including perioperative units, interventional radiology, cardiac catheterization labs, dialysis units—that weren’t historically part of the plan. For example, patients who are “boarding” in the ED on a stretcher for hours or even days require the same skin protection as those who’ve been admitted to an inpatient bed. And those in the OR who are anesthetized and unable to reposition themselves are at risk for PIs. Decreases in perfusion are cumulative, and they’re perpetuated across care settings when adequate perfusion isn’t assured. A skin injury that begins in the ED can be exacerbated in the OR and then appear as a PI in the critical-care unit. Patients need pressure redistribution and tissue off-loading in all care settings.
This special report takes all of these patient, team, and environmental factors into account and describes best practices, tools, and solutions for skin safety. I want to thank the thought leaders who shared their wisdom in creating this body of knowledge. The authors describe the current state of PIs and their assessment and prevention as well as strategies used to mitigate risk across a variety of acute-care settings. They also share best practices for multidisciplinary collaboration across settings to ensure that prevention practices are sustained as patients transfer from one area to another. In case studies, you’ll learn how clinical experts have explored a variety of approaches and solutions that you can put into practice tomorrow.
You’ll also find discussions on technology solutions and strategies for making the business case to acquire the technology needed to support your PI-prevention initiatives.
The many spokes on the PI prevention wheel must be in full gear to create an effective and sustainable program. As patient needs and acuity escalate, clinical excellence and patient advocacy will be more important than ever. Industry experts can play an important role as your partners in clinical quality and patient safety. At Dabir, our mission is to be your partner as you create evidence-based practice environments and teams that prevent PIs and enhance patient outcomes. We hope that this special report will assist you and your teams in these efforts and provide you the best solutions and approaches to PI prevention.
Melissa A. Fitzpatrick is vice president and chief clinical officer at Dabir, Inc., the healthcare division of Methode Electronics.
Selected reference
Black JM, Edsberg LE, Baharestani MM, et al; National Pressure Ulcer Advisory Panel. Pressure ulcers: Avoidable or unavoidable? Results of the National Pressure Ulcer Advisory Panel Consensus Conference. Ostomy Wound Manage. 2011;57(2);24-37.
ANT0518_Dabir_Intro