Opioids provide superb pain relief and are among the least expensive drugs prescribed. Plus, in low doses, they’re usually safe.
But these potent analgesics do pose dangers. The risks of abuse and serious adverse effects have always come with the benefits of opioids. Now, based on new information from the Institute for Safe Medication Practices (ISMP), the Food and Drug Administration (FDA), and the Joint Commission, there’s a growing awareness of safety concerns.
New safety recommendations
Because of a controversy regarding the use of opioids for chronic, persistent noncancer pain, the American Pain Society and the American Academy of Pain Medicine issued a new guideline in 2009. The guideline panel, a multidisciplinary group of national experts, performed a systematic review of the pertinent literature and made the recommendations summarized below.
- Before starting long-term opioid therapy, obtain a health history and perform a physical examination to assess the patient’s potential for opioid abuse. Obtain informed consent.
- Consider initial treatment with opioids to be a therapeutic trial. Analyze the risks and benefits and individualize the dosage, especially if the patient has moderate to severe pain that adversely affects the quality of life.
- Clinicians familiar with the use and risks of methadone should initiate a patient’s methadone therapy.
- Carefully monitor all patients using long-term opioid therapy. Monitor patients who have a history of aberrant drug-related behaviors closely—for example, by using more frequent urine screening.
- Anticipate adverse effects and assess patients for changes in opioid requirements, dosage escalations, and compliance with opioid therapy. If a patient experiences adverse effects or decreased pain relief, consider rotating several opioids to achieve better pain relief.
- Use a multidisciplinary approach to opioid therapy that includes psychotherapeutic options (such as cognitive behavioral therapy, progressive relaxation, and biofeedback), functional restoration, and interdisciplinary therapy. When patients repeat aberrant drug-related behaviors, engage in drug diversion, or aren’t progressing toward therapeutic goals, opioid therapy may be discontinued; when patients have intolerable adverse effects, the dosage or the opioid may be changed.
- Counsel patients not to drive when impaired and not to take opioids during pregnancy.
- Every patient using long-term opioid therapy should have a primary clinician who oversees medical care.
The recommendations include using these tools and screening instruments to determine the risk to the patient:
- Screener and Opioid Assessment for Patients with Pain (SOAPP)
- Diagnosis, Intractability, Risk, Efficacy (DIRE)
- Opioid Risk Tool (ORT)
- Current Opioid Misuse Measure (COMM)
- Pain Assessment and Documentation Tool (PADT).
Variable responses
Common opioids include morphine, oxycodone, codeine, hydrocodone, hydromorphone, fentanyl, meperidine, and methadone. These drugs bind to mu receptor sites throughout the central and peripheral nervous systems to produce analgesia. How-ever, recent research reveals that numerous alleles of the mu receptor gene and numerous receptor subtypes can create differences in opioid binding ability, affecting analgesia.
These genetic differences help explain some of the variation in response to opioids and opioid doses. The two biggest influences on opioid efficacy for pain relief are genetic polymorphism at the mu binding sites and variations in opioids. (See Opioid responses: The role of genetics.)
Other factors that can influence opioid metabolism and affect analgesia include:
- the CYP450 system in the liver, which transforms some opioids into usable metabolites
- the metabolism rate of opioids, which may be poor, intermediate, extensive, or ultrarapid
- racial differences (5% to 10% of White people are unable to or have a poor ability to metabolize codeine to morphine, the active metabolite).
To keep therapy safe despite these variables, ask the patient or family members about past experiences with opioids. Did a small dose control pain? Or did the patient need a large dose? Did the patient become oversedated? The answers will provide a baseline for selecting the analgesic and the dosage.
If the patient has never had an opioid, carefully monitor his or her response. The dosage may need to be titrated to achieve safe, effective pain relief.
Getting it right
Since including pain management in the Joint Commission standards in 2001, the Commission has focused on these areas: adequate pain management, pain assessment, drug use, and sentinel events related to drug use. The Joint Commission has also developed Patient Safety Goals that include goals for safe drug use summarized below:
- Be alert for drug names that look alike or sound alike, such as MS Contin, which is extended-release morphine, and OxyContin, which is extended-release oxycodone.
- Maintain a list of high-alert drugs and provide methods for decreasing confusion, such as “TALL man” lettering for drug names—for example, MORphine and HYDROmorphone.
- Avoid confusing abbreviations, such as “QD” for “every day.”
- Make sure all patient drugs are checked on admission and current drugs are reviewed by the physician daily.
Data from the Medications Errors Reporting Program and U.S. Pharmacopeia (USP) MEDMARX data indicate that opioids, particularly morphine and hydromorphone, are among the most frequently confused high-alert drugs—that is, drugs with a high risk of patient harm when an error occurs. In 2003, I.V. opioids were among the top 10 high-alert drugs.
Risky opioids
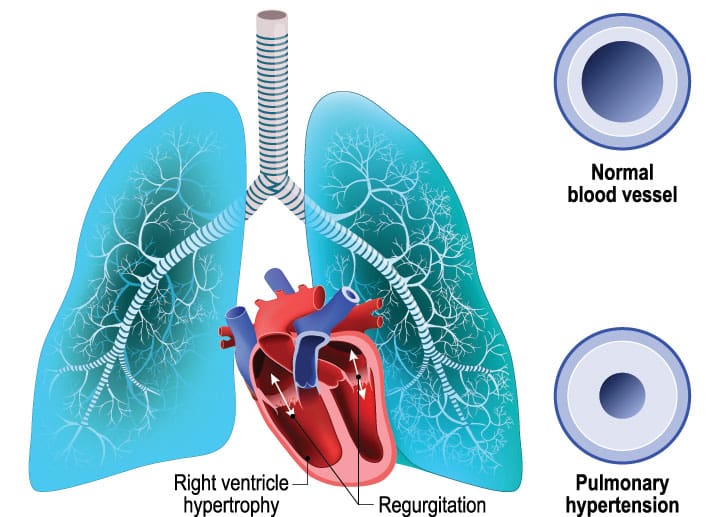
All opioids can cause oversedation and respiratory depression, but some are more problematic than others. Meperidine (Demerol) has a metabolite called normeperidine that can build up in the central nervous system (CNS) and cause seizures. For this reason, meperidine is no longer considered a first-line drug for pain.
Propoxyphene N-100 contains 650 mg of acetaminophen and a small amount of propoxyphene (Darvocet), which has a cardiotoxic metabolite that can cause cardiac arrhythmias or seizures. The FDA is considering removing this drug from the market.
The neuroexcitatory adverse effects of meperidine and propoxyphene are related to CNS sensitivity and renal insufficiency and thus more common in older patients and patients with renal impairment. Neither drug should be used in elderly patients.
Methadone can be used for chronic pain. However, because a dose provides analgesia for only 6 to 8 hours and estimates of the drug’s half-life range from 12 to 120 hours, methadone poses a high risk of delayed respiratory depression. The drug also can cause torsades de pointes, a cardiac arrhythmia, when used at high doses over time.
All patients taking methadone on a regular basis should have regular electrocardiograms to detect cardiac abnormalities. Pain therapy should start with short-acting drugs before a patient uses the longer-acting methadone. After the switch to methadone, carefully monitor the patient for sedation and respiratory failure. Monitor dosage increases, which should occur no sooner than every 3 days because of the drug’s long half-life.
Problems with patient-controlled analgesia
Patient-controlled analgesia (PCA) was developed as a means of increasing pain relief and patient satisfaction with pain control after surgery. Using a pushbutton, a patient can activate a portable pump containing a reservoir of a prescribed analgesic. The pump is programmed to give no more than the prescribed amount. Both the American Society of Anesthesiologists and the American Society of PeriAnesthesia Nurses endorse the use of PCA for postoperative pain relief. (See Patient-controlled analgesia vs. intermittent injections.)
However, overdoses in patients using PCA have raised safety concerns. One of the main reasons for the adverse reactions has been incorrect programming of the PCA pump.
Common programming errors include:
- delivering a bolus dose and then forgetting to return the pump settings to the correct rate
- confusing “milligram” and “milliliter”
- selecting the wrong lockout
- selecting the wrong drug concentration
- confusing “PCA bolus dose” with “PCA basal dose.”
PCA continuous infusions are no longer recommended for opioid-naïve patients because they add little analgesia but create a high risk of oversedation. PCA by proxy, use of the PCA device to deliver a drug dose by an unauthorized person, can produce serious, sometimes fatal, outcomes. The medication error database for the USP lists 6,069 PCA errors; 460 of them resulted in harm or death. PCA by proxy was responsible for 12 of these errors. One death resulted from a nurse activating the PCA button for patients.
To use PCA safely, the ISMP and the Joint Commission recommend the following:
- Determine which patients are good candidates for PCA. Don’t select patients who can’t activate the PCA pump independently, such as confused patients and patients who don’t understand how to activate the dose mechanism.
- Use two independent nurse checks to confirm the PCA rate, drug, concentration, and dose settings.
- Clearly identify where each I.V. line is infusing.
- Use prefilled syringes or bags.
- Use standardized order sets.
When monitoring PCA therapy, assess the patient for oversedation and hypoventilation. Using a simple scale such as the Ramsey sedation scale can help you identify the onset of sedation. Simply rousing a patient isn’t reliable. A patient who is starting to experience oversedation can be awakened and respond to questions and then quickly return to an oversedated state.
Capnography, which measures the build-up of carbon dioxide in the blood, can detect hypoventilation, a good indicator of impending respiratory depression. Relying only on oxygen saturation readings can be deceiving because supplemental oxygen can skew the readings. If you regularly monitor the patient’s respiratory rate and depth and sedation levels, PCA can be a safe, effective way to control pain.
Misuse of the fentanyl patch
The fentanyl patch (Duragesic) is a transdermal drug system that provides constant delivery of the opioid fentanyl. The system creates a drug depot in the dermal layers from which the drug can be delivered into the bloodstream at a consistent rate. The patch can take up to 18 hours to consistently deliver the prescribed dose. Achieving steady state in the patient’s blood can take up to 48 hours. This delayed action can cause delayed respiratory depression.
In the United States, more than 100 patients have died from overdoses related to fentanyl patches. These deaths resulted from poor understandings of how the patch works and which patients should use it. Because of its delayed effect, the patch isn’t indicated for acute pain. Also, before using the patch, patients should be receiving opioids regularly.
Patients who haven’t been receiving I.V. or oral opioids should be given other, shorter-acting types of analgesics, not the fentanyl patch. As the prescribing information for fentanyl notes, even opioid-tolerant patients can become oversedated with large doses.
Teach patients using fentanyl patches these safety points:
- Don’t cut the patch. Doing so can result in an overdose.
- Don’t apply heat over the patch.
- Dispose of the patch by folding the adhesive side, so it sticks to itself. Then, place it safely in a closed container or flush it down the toilet.
- Don’t place the patch in a regular wastebasket.
Safety considerations
As a nurse, you’re in a good position to make a judgment about a patient’s ability to comply with the drug order as written. Some patients don’t understand how to take drugs or will stop taking them when adverse effects occur. To avoid misunderstandings, at each visit or admission, observe how patients are taking their drugs, count how many tablets they’ve used, and look for outdated drugs and remove them. These actions will go a long way toward making sure patients take their drugs correctly.
To make opioid therapy safe, make sure you take these steps:
- Become familiar with opioid drugs and common dosages.
- Locate good resources, such as pain specialists or pharmacists, who can provide information about using opioids correctly.
- Know the signs and symptoms of opioid toxicity.
- Be aware that using drugs with sedative effects, such as antiemetics, muscle relaxants, and sedatives, increases the risk of oversedation.
- Teach patients the reason they are taking opioids, the prescribed dose, and the possible adverse effects. Give patients a phone contact in case adverse reactions develop.
- Maintain competency in entering PCA prescriptions and machine programming.
- If PCA therapy is being considered, make sure your patient is a suitable candidate.
- Use a sedation scale to monitor patient response to opioids.
- Monitor patients starting opioid therapy every 2 hours. (See Instituting safe opioid practices.)
Improving safety
Measures are being developed to help nurses and practitioners who prescribe and administer opioids. Bar-coding can help determine if the right drugs are being given to the right patients. Using drug reconciliation to check home drugs against prescribed drugs can identify errors in drugs and doses. The FDA is now calling for drug companies to formulate risk evaluation and mitigation strategies for opioids, so prescribers can make more informed drug choices based on the risks and benefits.
Avoiding the dangers of opioid therapy requires that prescribers, nurses, and patients have appropriate information on safe administration and dosages and potential adverse effects as well as expert contacts to call with questions and concerns. When you and your colleagues have the best information and use the best practices, your patients will reap analgesic benefit of opioids without encountering the dangers.
Selected references
American Pain Society. Principles of Analgesic Use in the Treatment of Acute Pain and Cancer Pain. 5th ed. Glenview, IL: American Pain Society; 2009:13,34.
Chou R, Fanciullo G, Fine P, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;
10(2):113-130.
D’Arcy Y. Pain Management: Evidence-Based Tools and Techniques for Nursing Professionals. Marblehead, MA: HcPro, Inc; 2007.
The Joint Commission. Focus on five: preventing patient-controlled analgesia overdose. Jt Comm Perspect Patient Saf. 2005;5:11.
U.S. Food & Drug Administration. FDA public health advisory: safety warnings regarding the use of fentanyl transdermal (skin) patches. http://www.fda.gov/cder/drug/advisory
/fentanyl.htm. Accessed March 29,2009.
Visit www.AmericanNurseToday.com/journal for a complete list of selected references.
Yvonne D’Arcy is a pain and palliative care nurse practitioner at Suburban Hospital in Bethesda, Maryland. The planners of this CNE activity have disclosed no relevant financial relationships with any commercial companies pertaining to this activity. The author is a speaker and an advisory board member for Endo Pharmaceuticals and Pfizer, a consultant and an advisory board member for Ortho-McNeil, and a writer for Abbott.