YOU MIGHT be wondering: Since when do nurses make laboratory errors? Actually, we make them fairly often—typically by using improper technique when collecting and handling samples and specimens. Preanalytic errors (those occurring before the sample or specimen is analyzed) account for 60% to 75% of all lab errors. These errors happen before the specimen even reaches the laboratory, usually during collection. They can lead to incorrect laboratory values with a potentially serious impact. For instance, they can result in a misdiagnosis and inappropriate treatment, leading to a life-threatening condition.
Some studies have found higher error rates in blood samples collected by nurses and other non-laboratory personnel, especially in the emergency department. This happens not from nurses’ lack of ability but from their lack of knowledge of and adherence to laboratory collection practices. Many factors must be considered during blood collection, so the chance of error is high unless nurses are well educated about the procedure. Common errors in blood sample collection include incorrect identification, wrong tube, insufficient sample quantity, clotting, hemolysis, and contamination.
Incorrect identification
Unlike some other errors, mislabeling of blood samples is 100% preventable. Consequences can be catastrophic if the labeling error goes undetected; in some cases, the patient may receive the wrong blood in a transfusion. Fortunately, the solution is simple: Positively identify the patient and apply the correct sample labels. And never let unlabeled samples or specimens leave the patient’s bedside.
Wrong tube, insufficient sample, and clotting
Using the wrong tube, collecting an insufficient quantity, and blood clotting can lead to delays in care and erroneous lab values. Electronic systems that generate labels specifying which type of tube to use can virtually eliminate wrongtube errors. Otherwise, consult with the laboratory if you’re unsure which tube to use.
Also, fill tubes with the recommended blood volume. This is especially critical with blue-top tubes used for coagulation studies, because accurate results hinge on the blood-sodium citrate ratio. Transfer blood from syringes to tubes promptly and gently invert the tube 8 to 10 times to ensure blood is mixed with the additive and to prevent clotting. For a summary of key actions to prevent these errors, see Preventing blood-collection errors.
Hemolysis
Numerous studies have investigated the causes of blood sample hemolysis, but findings are somewhat contradictory. Many studies concluded that compared to peripheral blood draws, blood withdrawn through an I.V. catheter is more likely to lead to hemolysis. But other studies found no difference, and the vast majority of samples drawn by I.V. catheter (more than 93% in most studies) are not hemolyzed. In light of this success rate, plus certain clinical factors (such as patient anxiety and discomfort, as well as the nurse’s risk of a needlestick injury), obvious reasons exist for drawing specimens from I.V. catheters.
Nonetheless, take additional steps to mitigate risk by using other hemolysis-reducing strategies as well. (See Avoiding blood-sample hemolysis.) For instance, keep in mind that red blood cells are fragile, so try to decrease the physical forces transmitted to blood at every step of the process. If you encounter resistance or turbulence when withdrawing blood, reposition the needle or catheter slightly to improve the flow. If this doesn’t work, consider discarding that blood sample and changing your phlebotomy technique.
Many clinicians believe certain types of equipment can increase hemolysis risk, but conflicting evidence exists on the effects of needle gauge, syringes vs. vacuum tubes, low (partial) vacuum tubes, and pneumatic tube systems to transport specimens. Be aware that drawing blood through an I.V. extension set or a needleless connector hasn’t been shown to increase hemolysis. Clearly, no single solution exists for blood-sample hemolysis, so be sure to use a multifactorial approach.
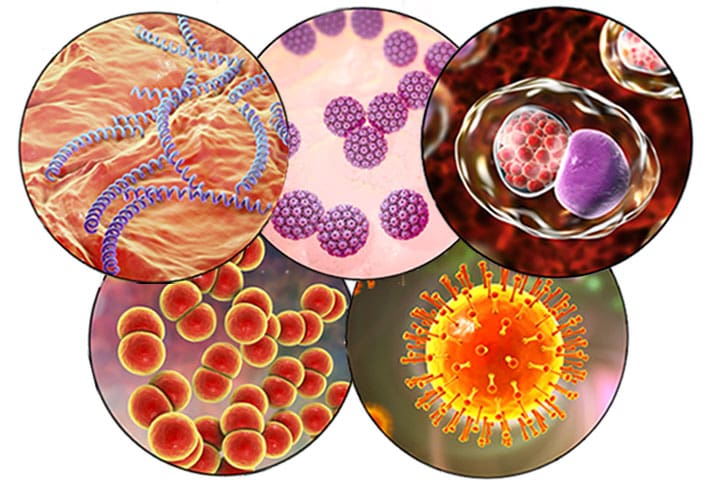
Blood-culture contamination
Each year, more than 1 million blood cultures in the United States are contaminated or produce falsepositive results. Contamination may lead to incorrect diagnoses and inappropriate patient care, increased morbidity and mortality, billions of dollars in additional testing, unnecessary antibiotic therapy, and extended hospital stays. Longer stays, in turn, increase patients’ risks for additional healthcare-related errors or complications. Inappropriate antibiotic use exposes patients to potential adverse effects, including development of drug-resistant organisms.
Contaminants can arise from equipment or the patient’s skin, so be sure to clean both. First, wash your hands and assemble supplies. Then scrub the tops of culture bottles with alcohol and let them air dry. Next, find the venipuncture site and clean the skin, using alcohol or a chlorhexidine-alcohol solution; both prevent blood-culture contamination more effectively than other skin-preparation solutions. Scrub the skin vigorously for 30 seconds and let it air dry completely for maximum effect. Unless you’re wearing sterile gloves, don’t palpate the site after it’s prepped. (See Preventing blood-culture contamination.)
Skin cells can enter the sample from the hollow-bore needle puncture of the skin, causing contamination. To avoid this, divert the first 1 to 2 mL of blood away from the culture bottle with a discarded syringe or plain vacuum tube (the top of which has been prepped with alcohol).
The needle used for venipuncture can cause contamination if it’s used to inoculate the culture bottles. Changing needles before inoculation increases the risk of needlestick exposure, so instead use equipment that lets you draw the sample directly into the culture bottle.
Bacteria colonize I.V. catheters rapidly after insertion. Avoid drawing blood-culture samples from a preexisting vascular access device unless the device itself is a suspected infection source. However, know that studies show blood can be withdrawn through a newly inserted peripheral I.V. catheter without increasing contamination. Don’t use newly inserted central venous catheters to collect blood cultures because these have been associated with an increased contamination rate.
Limiting blood-culture collection to dedicated phlebotomy staff also has been effective in reducing contamination and decreasing costs and risks associated with contaminated cultures. Other interventions that show promise in reducing contamination are procedural checklists, use of a sterile field, routine use of sterile gloves, and prepackaged supply kits.
Collaboration is key
The chain of events used to obtain accurate laboratory test results is long—and only as strong as the weakest link. Collaborate with laboratory personnel to implement an improvement plan that addresses both individual and departmental performance. To help ensure nursing isn’t the weakest link, nurses should receive thorough phlebotomy education and training, performance monitoring, and feedback about laboratory errors, especially hemolysis and blood culture contamination.
Jean A. Proehl is an emergency clinical nurse specialist with Proehl PRN, LLC, in Cornish, New Hampshire. She also works per diem as an emergency nurse at Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, and Gifford Medical Center in Randolph, Vermont.
Selected references
Alahmadi YM, Aldeyab MA, McElnay JC, et al. Clinical and economic impact of contaminated blood cultures within the hospital setting. J Hosp Infect. 2011;77(3):233-6.
Dawson S. Blood culture contaminants. J Hosp Infect. 2014;87(1):1-10.
Kelly AM, Klim S. Taking blood cultures from a newly established intravenous cathe ter in the emergency department does not increase the rate of contaminated blood cultures. Emerg Med Australas. 2013;25(5):435-8.
Lippi G, Banfi G, Church S, et al; European Federation for Clinical Chemistry and Laboratory Medicine Working Group for Preanalytical Phase. Preanalytical quality improvement. In pursuit of harmony, on behalf of European Federation for Clinical Chemistry and Laboratory Medicine (EFLM) Working group for Preanalytical Phase (WG-PRE). Clin Chem Lab Med. 2015;53(3):357-70.
Lippi G, Caola I, Cervellin G, et al. Error rates during blood collection in emergency departments and outpatient clinics: results of a prospective multicenter study. Clin Chim Acta. 2015;445:91-2.
Lippi G, Cervellin G, Mattiuzzi C. Critical review and meta-analysis of spurious hemolysis in blood samples collected from intravenous catheters. Biochem Med (Zagreb). 2013;23(2):193-200.
Patton RG, Schmitt T. Innovation for reducing blood culture contamination: initial specimen diversion technique. J Clin Microbiol. 2010;48(12):4501-3.
Proehl JA, Bradford JY, Leviner S, et al. Clinical practice guideline: Prevention of blood specimen hemolysis in peripherally-collected venous specimens. Des Plaines, IL: Emergency Nurses Association; 2012.
Proehl JA, Leviner S, Bradford JY, et al. Clinical practice guideline synopsis: Prevention of blood culture contamination. Des Plaines, IL: Emergency Nurses Association; 2012.
Septimus E. Clinician guide for collecting cultures. Reviewed and updated April 7, 2015. Centers for Disease Control and Prevention.
Stohl S, Benenson S, Sviri S, et al. Blood cultures at central line insertion in the intensive care unit: comparison with peripheral venipuncture. J Clin Microbiol. 2011;49(7):2398-403.
Wollowitz A, Bijur PE, Esses D, Gallagher EJ. Use of butterfly needles to draw blood is independently associated with marked reduction in hemolysis compared to intravenous catheter. Acad Emerg Med. 2013;20(11):1151-5.