Nearly 6 million Americans suffer from heart failure (HF). The American Heart Association predicts that the number of individuals diagnosed with HF will increase 46% by 2030. HF can’t be cured, but it can be managed with medications—until it reaches an advanced stage. At that point, a heart transplant or an implanted left ventricular assist device (LVAD) is the only long-term option for survival.
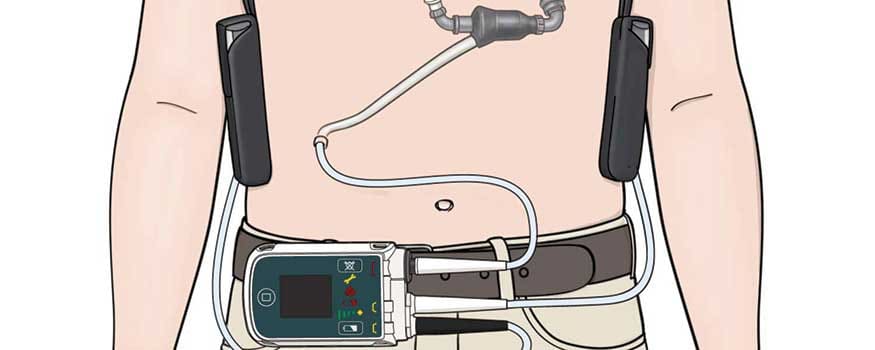
A continuous-flow pump, the LVAD directs blood from the left ventricle to the ascending aorta. (See Understanding the LVAD.) The Food and Drug Administration FDA) first approved the LVAD for patients waiting for heart transplants; when used for this purpose, the device is considered a bridge to transplant. While a heart transplant is optimal, demand for donor hearts far exceeds supply. For that reason, LVADs have become increasingly popular as a destination therapy. The HeartMate II® by Thoratec is the only FDA-approved LVAD for destination therapy.
Since 2006, more than 20,000 patients have received LVADs as destination therapy, and this number is expected to increase. For this reason, nurses need to become more knowledgeable about—and confident in—caring for patients with these devices. This article discusses nursing care of patients with LVADs for destination therapy, including device and medication management, potential complications, patient education, and psychosocial support for patients, home caregivers, and nurses.
Myocardial infarction: Nursing assessment and care
Managing acute decompensated heart failure
Attacking anterior-wall myocardial infarction in time
Who benefits from an LVAD?
Although no stringent patient-selection guidelines exist, a provider usually refers a patient for an LVAD when advanced HF no longer responds to inotropic drugs or surgical interventions, such as valve repair. Patient evaluation for an LVAD includes nutritional status, end-organ function, right ventricular function, and signs or symptoms of infection. Patients also should be screened for depression and other psychological problems.
The selection process includes determining if a home caregiver is willing and able to care for the patient around the clock for at least 3 to 6 months after surgery. Home caregivers must learn how to care for the device and assist patients. Caregiver responsibilities include helping patients manage their LVAD, monitoring for infection, changing driveline dressings, managing medications, assisting with activities of daily living, and providing transportation to and from medical appointments. Depending on the patient’s needs and whether complications occur, caregiving may be needed for the rest of the patient’s life.
Approval for an LVAD typically occurs over several meetings between the patient and family and a team consisting of a cardiologist, a cardiothoracic surgeon, an LVAD (or VAD) coordinator, a social worker, and a palliative care provider. Many VAD coordinators are RNs who have special training in these devices. Based on the team’s recommendation, the cardiothoracic surgeon will ultimately decide if the patient is a candidate for an LVAD.
Proper assessment
Caring for the hospitalized patient with an LVAD begins with a thorough assessment of both the patient and LVAD.
Monitor blood pressure and mean arterial pressure (MAP); the goal is 60 mm Hg to 90 mm Hg. Elevated MAP decreases flow and perfusion. If MAP is too high, the patient may require antihypertensive drugs, such as metoprolol, hydralazine, and isosorbide dinitrate. These drugs may need to be adjusted until the goal MAP is reached. Always check with the provider before holding any medications due to a low MAP.
Check the LVAD each time you assess the patient’s vital signs. You will hear the continuous humming sound of the pump when auscultating the heart. Make sure the battery-charging station is plugged into the wall and at least two spare batteries are in the charge station; a green light indicates a full charge. Additional safety checks include assessing the driveline to ensure it’s securely in place and confirming there’s a backup system controller in the room.
The LVAD may be connected to the power module, which is plugged into the wall; or, to allow more mobility, the patient may wear the batteries in a holster. When the device is plugged into the module, several numbers on the system monitor indicate pump flow, pump speed, pulse index, and power. (See The 4 Ps of the LVAD.) If the patient is wearing a battery holster, the numbers must be read from the controller.
Technical care of the LVAD
The LVAD requires regular care and system checks, including power-source changes, daily self-tests, and driveline dressing changes. Performing these tasks in the hospital provides teaching opportunities for patients and caregivers. (See Essential education for patients and caregivers.)
Switching power sources
Patients and caregivers can learn how to change between batteries and the power module by watching you do it, so try to do it the same way every time. For example, always change out the white power cables first and then the black.
To change from one power source to the other, push the connectors of the white cables together and turn counterclockwise to disconnect. To reconnect, align the half moons on the connectors, push them together, and turn clockwise until they’re flush. Repeat the same steps with the black cables. Think “power, patient, power” to remind yourself to disconnect and reconnect one power source at a time.
Never disconnect both sets of cables at the same time; this essentially leaves the patient without a power source. The system controller provides power for a limited time, but never rely on it. Tell the patient the device will sound an alarm when changing between power sources.
Performing a daily self-test
Teach the patient to perform a daily self-test to ensure the LVAD is working properly. When the patient presses and holds the battery button on the system controller, the screen displays “Self Test.” If the panel is working properly, the audio alarm will sound and control panel alarms will light up. These alarms include power and battery alarms, a red heart (hazard) alarm, and a wrench (advisory) alarm.
Changing the driveline dressing
Assess the driveline site during each patient assessment, or more frequently if you’re concerned about dislodgment. Except under special circumstances, the driveline dressings must be changed daily or every other day, depending on the provider’s order and how long the patient has had the LVAD. (See How to change a driveline dressing.)
Ultimately, you’re responsible for ensuring the dressing change is completed; however, if you or the VAD coordinator have trained and observed the patient and caregiver changing the dressing, you can let them do it.
Medication management
Patients with LVADs are typically prescribed several medications, including anticoagulants, antiplatelet agents, antihypertensives, antiarrhythmics, fluids, and electrolytes.
Anticoagulants and antiplatelets
Anticoagulants and antiplatelets (for example, heparin, warfarin, and aspirin) help prevent pump thrombosis. However, these drugs increase hemorrhage risk.
Antihypertensives
Adequate blood pressure (typically, a MAP between 60 mm Hg and 90 mm Hg) helps maintain sufficient pump flow. Commonly prescribed antihypertensive drugs include:
• vasodilators, such as hydralazine and isosorbide dinitrate
• beta blockers, such as metoprolol and carvedilol
• angiotensin-converting enzyme (ACE) inhibitors, such as lisinopril.
Always monitor heart rate and blood pressure when giving these medications.
Fluid and electrolyte replacement
Most patients with HF are restricted to 2 L of fluid per day. For patients with LVADs, who depend on adequate volume and pressure to maintain flow, you may need to push fluids to achieve the best filling pressures. For patients with long-term HF, provide education to ensure they don’t become dehydrated after receiving the device.
The decision to push fluids depends on the patient’s hemodynamic status. Signs of compromised fluid status include decreased pump flow and pulse index, as well as increased hemoglobin and hematocrit. Common indications of fluid overload, which can lead to right ventricular failure, include weight gain, edema, and shortness of breath, all of which indicate increased preload.
Keeping electrolytes, such as potassium, magnesium, sodium, and calcium, within normal ranges helps prevent arrhythmias. Check your patient’s basic metabolic panel, comprehensive blood count, prothrombin time, and international normalized ratio (INR) daily.
Managing complications
Common LVAD complications include infection, pump thrombus, hemorrhage, arrhythmias, and suction events.
Infection
Several factors put patients with LVADs at high risk for infection—for example, malnutrition. Potential sources of infection include ventilators, central venous catheters, peripheral I.V. lines, and indwelling urinary catheters. Keep in mind that all hospital patients are at risk for methicillin-resistant Staphylococcus aureus infection and Clostridium difficile infection, as well as pressure injuries, which can become infected.
After surgery, driveline infections are common. To help prevent these infections, provide thorough patient and caregiver education on performing driveline dressing changes.
Pump thrombus
Signs and symptoms of pump thrombus include increased heart rate, shortness of breath, increased pulse pressure, and a steady increase in pump power over several days. If the pump is completely occluded by a clot, the pump flow rate decreases. Notify the provider immediately if the patient experiences any of these problems. Treatment of pump thrombus involves anticoagulant or antiplatelet therapy, direct infusion of a local thrombolytic into the LVAD, or pump replacement. To avoid these problems, monitor lab values to help ensure the patient’s INR is in the therapeutic range, typically 2 to 3.
Hemorrhage
Lifelong anticoagulant use puts patients at risk for hemorrhage, especially stroke or GI bleeding. Signs and symptoms of GI bleeding are frank red to black tarry stools, a significant drop in hematocrit, decreased oxygen saturation, pallor, and dizziness. Anticoagulant therapy may need to be adjusted, and the patient may require blood products.
Suction event
A suction event occurs when pressure inside the ventricles drops too low, causing the internal cannula to adhere to the left ventricular septum. This typically results from hypovolemia. Other causes include high pump speed and poor internal cannula positioning. A suction event isn’t life-threatening in itself but can lead to ventricular arrhythmias, such as ventricular tachycardia. Notify the provider immediately if you suspect a suction event.
Treatment may include pushing fluids to restore ventricular pressure, treating the cause of hypovolemia (such as over-diuresis or GI loss), or surgery to restore proper cannula positioning.
Arrhythmias
Arrhythmias, such as ventricular tachycardia and atrial fibrillation, are common in LVAD patients. Many of these patients had a pacemaker placed before surgery to treat atrial fibrillation. After LVAD placement, arrhythmias are medically managed with antiarrhythmic agents, such as amiodarone and digoxin. For a newonset arrhythmia, assess the patient to see if he or she is stable or symptomatic, check electrolyte levels, and notify the provider.
Contact the provider and VAD coordinator immediately if the patient experiences symptomatic or sustained ventricular tachycardia (longer than 30 seconds) or ventricular fibrillation. If the patient becomes unresponsive, call a code blue. Avoid chest compressions except as a last resort because they can dislodge the LVAD andcause irreparable damage. Give medications per advanced cardiac life support protocol. You can leave the pump running during defibrillation.
Psychosocial support
Patients with LVADs experience many physical and emotional changes. Although there are many physiological benefits (increased energy, reduced shortness of breath), patients may become depressed or even suicidal. Many patients feel socially isolated and express frustration over loss of control and dependency on family and caregivers. Others may be afraid of their device.
Assess patients for depression on admission and throughout their hospital stay. Ask how they’re managing daily life using open-ended questions, such as:
• How has your life changed since receiving an LVAD?
• What are your greatest concerns after leaving the hospital?
• How will you cope with these concerns?
• What are some benefits and challenges you’ve experienced since receiving your LVAD?
Teach coping skills, such as journaling, meditation, art therapy, prayer, and the importance of reaching out to others. Patients with LVADs can offer significant support to one another, so provide information about support groups.
Caring for the home caregiver
Caregiving can be burdensome. Many caregivers express fear of the LVAD, regret taking on the role, or experience depression and anxiety. They need support, even if the patient has had an LVAD for a long time. Provide caregivers with resources for support groups where they can receive encouragement and respite care.
Self-care for the nurse
Many nurses who are new to caring for patients with LVADs express anxiety over caring for this patient population. Make sure you’re up-to-date with your employer’s standard education on LVADs. Refamiliarize yourself with the equipment and ask to shadow a nurse who’s caring for a patient with an LVAD. Ask for help from someone who’s more experienced. VAD coordinators are excellent sources of support, so find out who’s on call and how to reach him or her.
In many cases, nurses who care for patients with LVADs get to know them and their families well and may experience grief if a patient becomes seriously ill or dies. If you feel you’re experiencing grief or burnout, reach out to a trusted coworker, manager, or counselor. Spend days off doing something enjoyable, such as spending quality time with family, friends, or a pet. Treat yourself to a massage or a relaxing bath, go outside, take a yoga class, or meditate. Most important, never forget why you became a nurse.
Rewarding challenge
As the population of patients with advanced HF increases, nurses in all healthcare settings need to become familiar with the care of patients with LVADs, including device assessment and management, potential complications, and patient and caregiver education and support. Caring for the patient with an LVAD can be challenging, but it’s also immensely rewarding.
Heather Martonik is a registered nurse in the coronary care unit at the Pulse Heart Institute at Multi- Care Health System in Tacoma, Washington.
Selected references
Benjamin EJ, Blaha MJ, Chiuve SE, et al.Heart disease and stroke statistics—2017 update: A report from the American Heart Association. Circulation. 2017;135(10):e146-603.
Brouwers C, Denollet J, Caliskan K, et al. Psychological distress in patients with a left ventricular assist device and their partners: An exploratory study. Eur J Cardiovasc Nurs. 2015;14(1):53-62.
Bruce CR, Delgado E, Kostick K, et al. Ventricular assist devices: A review of psychosocial risk factors and their impact on outcomes. J Card Fail. 2014;20(12):996-1003.
Doty D. Ventricular assist device and destination therapy candidates from preoperative selection through end of hospitalization. Crit Care Nurs Clin North Am. 2015;27(4):551-64.
Hohner E, Crow J, Moranville MP. Medication management for left ventricular assist device thrombosis. Am J Health Syst Pharm. 2015;72(13):1104-13.
Jennings DL, Jones MC, Lanfear DE. Assessment of the heart failure pharmacotherapy of patients with continuous flow left-ventricular assist devices. Int J Artif Organs. 2012;35(3):177-9.
Magid M, Jones J, Allen LA, et al. The perceptions of important elements of caregiving for a left ventricular assist device patient: A qualitative meta-synthesis. J Cardiovasc Nurs. 2016;31(3):215-25.
Marcuccilli L, Casida JJ, Bakas T, Pagani FD. Family caregivers’ inside perspectives: Caring for an adult with a left ventricular assist device as a destination therapy. Prog Transplant. 2014;24(4):332-40.
Miller LW, Guglin M. Patient selection for ventricular assist devices: A moving target. J Am Coll Cardiol. 2013;61(12):1209-21.
Modica M, Ferratini M, Torri A, et al. Quality of life and emotional distress early after left ventricular assist device implant: A mixedmethod study. Artif Organs. 2015;39(3):220-7.
Ottenberg AL, Cook KE, Topazian RJ, et al. Choices for patients “without a choice”: Interviews with patients who received a left ventricular assist device as destination therapy. Circ Cardiovasc Qual Outcomes. 2014;7(3):368-73.
Park SJ, Milano CA, Tatooles AJ, et al. Outcomes in advanced heart failure patients with left ventricular assist devices for destination therapy. Circ Heart Fail. 2012;5(2):241-8.
Rommel JJ, O’Neill TJ, Lishmanov A, et al. The role of heart failure pharmacotherapy after left ventricular assist device support. Heart Fail Clin. 2014;10(4):653-60.
Thoratec Corporation. HeartMate II® LVAS clinical operation & patient management. 2011.
Thoratec Corporation. Proven alternative for advanced heart failure.


















8 Comments.
This is a FABULOUS resource for any nurse who cares for VAD patients. Also a great refresher!
My husband is an LVAD patient and it,s almost a year he had it. He’s doing really great with it. He didn’t have no alarms since he had it and I been caring for him since. My job is still on hold for me so I would like to know if I can go back to work. I am a caregiver and they maybe can give me 5 hours a day to work so can I go back to work?
I’m looking for a nurse to change my dressing on a daily basis in Houston Texas
Need help with care for a LVAD person. Need a nurse to come by the house since Medicare doesn’t provide long term rehab. This is in Springfield, MO
can you also tell me more about pulse index etc
i have an lvad i would like to know if they teach anything bout them or
the care of an lvad patient in nursing school
May I know what are the requirements/courses needed for a nurse to be able to care for patients on LVAD?
is there a specific course?
exam?
or a higher academic educational degree than a Bachelor degree?
your response is highly appreciated.
kind regards
I understand that there may not be a pulse with LVAD. What about a rhythm? Does the LVAD take over the heart much like a pacemaker and you see P&C? What kind of rhythm would one see if on a moitor?
To do vital signs, take the heart rate by listening to the heart? Does the LVAD have a range like a pacemaker?