Organize, communicate, and document for a successful clinical nursing instructor experience.
Takeaways:
- The transition from expert clinician to novice clinical instructor requires a shift in thinking.
- Today’s nursing programs are placing more emphasis on critical thinking and safe patient care using current best evidence.
By Melinda Bowman, MSN, RN, CNE, CMSRN
Congratulations! You’ve completed your master of science in nursing (MSN) and you’re about to accept your first position as an adjunct clinical nursing instructor. You’ll transition from being an expert clinician to a novice educator. This may seem intimidating, but don’t worry, many of your patient care skills—organization, patience, clear communication, and thorough documentation—will easily transfer. And familiar concepts, such as legal considerations and your role at the bedside, just require a shift in thinking. Because the more knowledge you have, the easier the transition will be, use these tips to get a successful start.
Organization: Before you begin
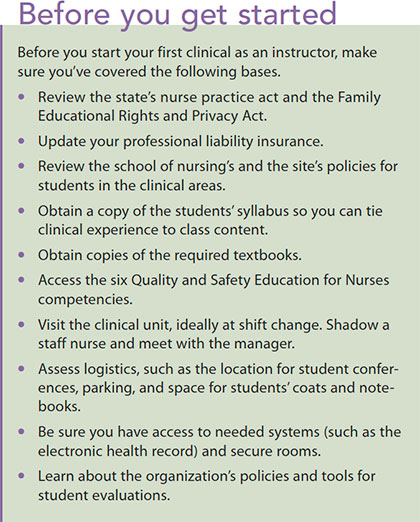 Ideally, you’ll be given a comprehensive orientation to the nursing program and access to all the course materials and resources that the students have, and you’ll be assigned to a seasoned faculty member to mentor you into your new role. If you’re not, don’t panic. Here’s a list of the minimum resources you’ll need and questions you’ll want answered. (See Before you get started.)
Ideally, you’ll be given a comprehensive orientation to the nursing program and access to all the course materials and resources that the students have, and you’ll be assigned to a seasoned faculty member to mentor you into your new role. If you’re not, don’t panic. Here’s a list of the minimum resources you’ll need and questions you’ll want answered. (See Before you get started.)
School policies
You should have access to all of the school’s policies for students in the clinical area. Make sure you know how many patients to assign and what the students can and can’t do under an RN’s supervision. You’ll also need a copy of the written objectives for the students’ clinical experience so you understand what the focus should be. Be aware that programs are placing less emphasis on tasks like bed baths and more emphasis on critical thinking.
Syllabus
To help you tie the students’ clinical experiences to class content, ask for the syllabus so you know what they’re learning in class each week. Note that the best time to link classroom concepts to the clinical area is the week after students have covered the content in class. You’ll want to know the theoretical content of the students’ classes, which should reflect current best evidence, so get copies of the main textbooks and ask the publishers for the digital editions.
QSEN competencies
If you’re not familiar with the six Quality and Safety Education for Nurses (QSEN) competencies, visit qsen.org. Review the knowledge, skills, and attitudes that should be instilled in undergraduate nursing students to improve the quality and safety of healthcare systems. Many nursing programs incorporate these competencies into their student learning outcomes and evaluation tools. Even if you haven’t heard of QSEN, you’ll already be familiar with the concepts the competencies cover.
Make a visit
Arrange to visit the unit where you’ll be working with students, preferably at change of shift so you can see how hand-off report is done. Shadow a staff nurse for a few hours to get a sense of the unit and its workflow.
Meet with the nursing manager to review the written objectives for the students’ clinical experience and ask for copies of the clinical policies for students. Discuss the best way to choose patient assignments and how they’ll be posted on the unit.
You’ll also want to ask for access to all systems and secure rooms before you begin. Other practical questions include where to find space for pre- and post-conferences, where students park, and whether the unit has a dedicated space for the students’ coats and notebooks.
Legal considerations
Your state nurse practice act, the school of nursing’s policies, and the clinical site’s policies will dictate what the students can and can’t do in the clinical area. Be sure you’re knowledgeable about each. Students aren’t practicing under your license, but they are practicing under your supervision for tasks that fall within the scope of practice for the degree that they’re seeking. They’re held to the same standard of practice as those with a license. Your job is to determine when students can safely function independently.
Consider an addition to your professional liability insurance that indicates you’re now teaching. Keep detailed written records, give timely feedback, and follow all policies so you can defend your professional decisions if a student sues.
Be aware of the Family Educational Rights and Privacy Act (FERPA), which protects students’ educational records. It also prohibits you from discussing a student’s progress with anyone who doesn’t play a role in that student’s education. Think of it as education’s Health Insurance Portability and Accountability Act.
Clear communication, thorough documentation
Everyone—you, students, nurse managers, and staff—must understand all requirements and expectations of the clinical experience. Be sure the manager and staff are aware of the students’ focus each week of clinical, and clearly communicate assignments and paperwork the students must complete, including how they’re submitted, who’s responsible for reviewing them, and the penalty for late submissions. Learn how you’re to give feedback to the students on their weekly performance, and consider keeping a written anecdotal record of each student’s clinical experiences and progress, even if it’s not required by the program. This record will be an invaluable resource when it’s time for formal evaluations.
 Make sure you know how and when students are to be formally evaluated. Ask to see completed examples of the evaluation tool, so you know how to structure your own evaluations. Understand what you’re to do if a student is unsafe or in danger of failing clinical, and communicate regularly with your lead course faculty about student progress.
Make sure you know how and when students are to be formally evaluated. Ask to see completed examples of the evaluation tool, so you know how to structure your own evaluations. Understand what you’re to do if a student is unsafe or in danger of failing clinical, and communicate regularly with your lead course faculty about student progress.
Clear communication with the students is equally important. Be clear about the learning objectives for each clinical day, and give students immediate feedback about how they’re meeting them. Remember to be respectful; feedback should be constructive and delivered in private.
Your new role at the bedside
One of the biggest role adjustments to make as you move from clinician to educator is to shift your thinking at the bedside. You’re a guest on the unit, there to guide the students’ learning. Resist the urge to step in and “do” if the patient deteriorates or the student stumbles. The primary RN is ultimately responsible for the patient’s care. Allow the student to struggle (safely) on his or her own to manipulate a piece of equipment or to come up with the answer to a patient’s question. Have patience. Remember, students are learning and it will take them what seems like a long time to complete tasks or make connections between theory and a patient’s presentation.
The transition from being an expert clinician to a novice educator may seem daunting. Many of the skills you already possess—organization, patience, and the ability to communicate clearly and document thoroughly—will serve you well. With these tips in mind, you’ll soon become as comfortable in your new role as you were in your old one.
Melinda Bowman is a nursing instructor at Our Lady of Lourdes School of Nursing in Camden, New Jersey.
ant4-Clinical instructor-322


















1 Comment.
Great article! Thank you for your tips to help transition from expert clinician to novice clinical instructor.