Strategies for implementing this policy change.
Takeaways:
- An organizational model for change is key to successful implementation of family presence during resuscitation.
- Nurses acting as change agents can lead a strategic plan with the goal of creating an ICU culture where family presence is a practice expectation.
By Carolyn Bradley, MSN, RN, CCRN; Janet Parkosewich, DNSc, RN, FAHA; Bertie Chuong, DNP, RN, CCRN
Most people know that resuscitation efforts aren’t always successful. Armed with this knowledge, family presence during resuscitation (FPDR) can be a comfort to patients who are fearful of dying alone without the support and advocacy of their loved ones. In addition, patients have a sense of relief knowing that their family will see that the resuscitation team did everything possible to save their lives. FPDR benefits the family as well by promoting transparency about life-saving measures. Witnessing resuscitation efforts reduces family members’ anxiety, minimizes feelings of patient abandonment, and provides comfort when they see the efforts made to revive their loved ones. However, not all patients want FPDR because of concern for family members and worry that they might distract the resuscitation team. Conversations with patients and families about FPDR will help allay concerns and highlight the potential benefits.
Implementing FPDR
FPDR is a patient- and family-centered care practice endorsed by the American Association of CriticalCare Nurses (AACN) and the Emergency Nurses Association (ENA). However, not all hospitals sanction it. And in settings that do offer FPDR, it’s not always fully implemented or practiced consistently.
The key to successful implementation of FPDR in the intensive care unit (ICU) is adopting a proven organizational model for change. Many models are available, but the one described by Kurt Lewin, a social psychologist, may be of interest to clinicians because it’s time-tested and easily applied in clinical settings. (See Lewin’s 3-step change model.) Change agents, who in the case of FPDR, are respected clinical experts, provide the leadership for this dynamic process.
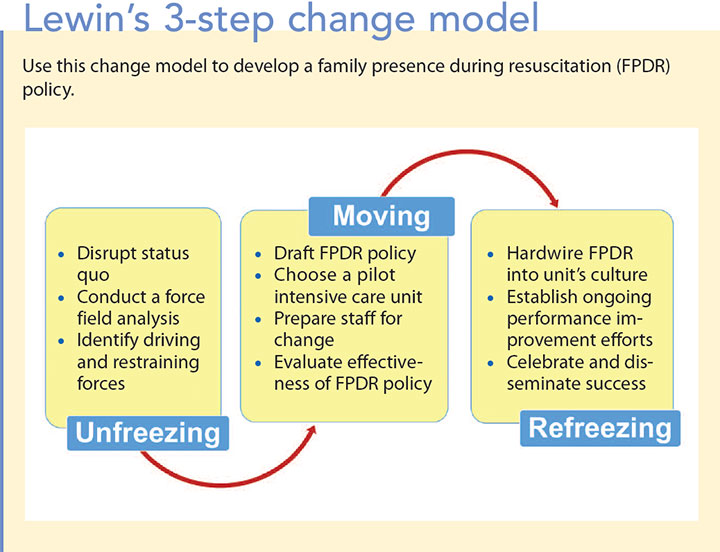
The process begins with the unfreezing stage, which disrupts the status quo and highlights the need for change. As a change agent, you’ll need to develop strategies to help people let go of sacred cows. When it comes to FPDR, nurses and other clinicians must recognize that sending families to the waiting room at the first sign of their loved one’s clinical deterioration is no longer acceptable.
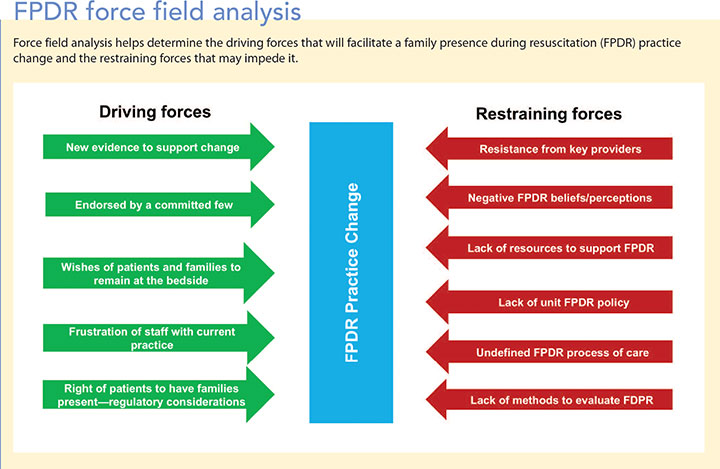
One critical aspect of unfreezing is force field analysis—a thoughtful critique of the current internal and external environments. (See FPDR force field analysis.) This analysis weighs the driving forces that will facilitate acceptance of a new practice, such as FPDR, against restraining forces that will undermine or impede the change. Overcoming restraining forces can be challenging because perceptions and beliefs may be embedded in the setting’s culture.
The moving stage involves planning, implementing, and managing the practice change, which can be introduced on a small scale and then refined based on feedback and evaluation. Most practice changes involve introducing new polices or practice guidelines, redesigning staff members’ roles and responsibilities, and providing education and skills training. Be persistent, keep a close eye on how well staff adhere to the new practice, engage those who embrace this change, and work to remove barriers.
The last step is the refreezing stage, which represents a shift in culture that wholeheartedly endorses the new practice and ensures that it’s applied consistently. You’ll need to work hard to realign the new policy with practice expectations, so establish processes for measuring adherence to the new practice and for providing clinicians with performance feedback.
Lewin’s 3-step change model in action
Use the following example of Lewin’s 3-step change model to integrate FPDR into your organization.
Unfreezing stage
First, confirm senior leadership support for FPDR. Key constituents include providers, nurse leaders, and others who make practice decisions. After support is confirmed, implement strategies to disrupt the status quo. The goal is to call attention to the need for FPDR in your ICU. Plant the seed for change by introducing the topic with clinical nurses, the nurse manager, other nurse leaders, and providers.
Disrupt the status quo
- Visit the ENA website with fellow clinicians to review the Clinical Practice Guideline for Family Presence during Invasive Procedures and Resuscitation. Review the AACN Practice Alert: Family Presence During Resuscitation and Invasive Procedures and other valuable resources.
- If your unit has a journal club, select a recent FPDR article for discussion.
- Use a recently published FPDR article, the ENA guideline, or AACN resources to have an informal conversation with colleagues so you can learn what they think about this practice.
- Use meeting time to invite guests from other units or hospitals that have successfully implemented FPDR.
Conduct a force field analysis
- Convene an FPDR steering committee to involve others in the change process. Interdisciplinary members can include nurses, providers, respiratory therapists, chaplains, social workers, child life specialists, patient and family advisors, and nursing assistants. Consider inviting individuals who support FPDR and those who resist.
Schedule regular meetings that encourage open, respectful dialogue about the positive and negative perceptions of FPDR. At the first meeting, discuss personal and professional discomfort about the practice. - Review the current evidence with the committee. Consider presenting case studies with FPDR best practices.
- Identify potential strategies to enhance driving forces and minimize restraining forces.
Moving stage
This phase involves interdisciplinary planning, piloting the new FPDR policy, and revising it as needed based on feedback.
Draft the FPDR policy
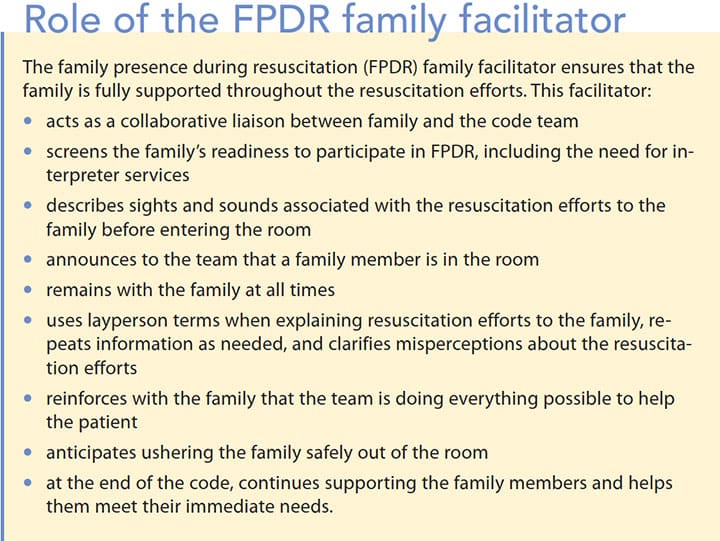
- Ensure that the policy provides clear guidelines and defines the roles of staff during FPDR, which includes details about the family facilitator role. (See Role of the FPDR family facilitator.) Delineate the process for documenting FPDR on the resuscitation electronic health record (EHR) flowsheet. The nurse’s role should include documenting whether FPDR was offered, if the family chose to be present, and if the family facilitator was present. This information will be useful for tracking policy adherence.
Choose a pilot ICU and prepare staff
- Identify a pilot unit that’s eager to lead the practice change. Unit leaders, providers, and clinical staff are all important stakeholders in deciding where the new practice will be piloted.
Select FPDR champions from those who truly endorse the practice. You want to choose individuals who will help to drive the change, and who are tenacious and uncompromising in their efforts to facilitate FPDR. They will assist in preparing the interdisciplinary team by providing FPDR education, training family facilitators, and communicating clinicians’ experiences with the steering committee. - Set a date to begin FPDR implementation.
Evaluate FPDR effectiveness during steering committee meetings
- Set standing agenda items that include FPDR champions’ feedback.
- Invite nurses, providers, and others to share their experiences.
- Conduct a balanced assessment of progress by examining barriers and highlighting examples of positive experiences.
- Establish communication processes to give positive feedback to team members who use FPDR and to find out why others have not routinely incorporated it into their practice.
- Implement plans to manage any barriers to effective FPDR.
- Revise the policy, as needed, while maintaining evidence-based standards.
 Refreezing stage
Refreezing stage
The refreezing stage sets in when FPDR becomes part of the ICU culture and clinicians no longer question its value. However, you’ll need to take actions during this stage to guarantee that FPDR is offered to every patient and family during every resuscitation. You, as the change agent, and FPDR champions should continue to drive this practice innovation and stay involved in all aspects of the refreezing stage.
Hardwiring FPDR into the unit culture
- Explore opportunities for senior leadership to demonstrate visible support for FPDR.
- Provide FPDR content during orientation of all appropriate new employees.
- Offer ongoing FPDR training and education.
- Establish a process that aligns employees’ performance evaluations with the FPDR unit initiative.
Ongoing performance improvement efforts
- Lead a performance improvement team to evaluate ongoing policy success.
- Establish process goals that measure how often: FPDR is offered to families, family members agree to participate at the bedside, and a staff member served as a family facilitator. Analyze EHR data to track these measures of success.
- Share stories from family members who experienced FPDR.
- Implement processes for timely performance data feedback to the FPDR steering committee, resuscitation team, and FPDR champions.
- Engage FPDR champions in providing performance data feedback to unit staff.
Celebrate and disseminate success
- Create a process for ongoing recognition of those who consistently demonstrate FPDR best practices.
- Disseminate your work to inspire others to embrace FPDR. Consider submitting abstracts for poster and podium presentations at local and national conferences. Work as a team to draft a manuscript for publication to share your FPDR journey.
Be the change
Changing your ICU’s culture to embrace FPDR requires a strategic plan, based on a proven theoretical approach. Visible senior leadership support, a committed change agent, focused FPDR champions, and engaged steering committee members keep the change process on track because they all share a common vision for the new policy. These strategies will methodically unfreeze current practice by disrupting the status quo, moving clinicians into accepting the need to pilot FPDR, and refreezing the ICU culture in which FPDR becomes a practice expectation.
The authors work at Yale New Haven Hospital in New Haven, Connecticut. Carolyn Bradley is a service line educator in the Heart and Vascular Center. Janet Parkosewich is the nurse researcher. Bertie Chuong is a resource and education coordinator in the Center for Professional Practice.
Selected references
American Association of Critical-Care Nurses. AACN practice alert: Family presence during resuscitation and invasive procedures. Crit Care Nurse. 2016;36(1):e11-4.
Batras D, Duff C, Smith BJ. Organizational change theory: Implications for health promotion practice. Health Promot Int. 2016; 31(1):231-41.
Bradley C, Keithline M, Petrocelli M, Scanlon M, Parkosewich J. Perceptions of adult hospitalized patients on family presence during cardiopulmonary resuscitation. Am J Crit Care. 2017;26(2):103-10.
Clark, AP, Guzzetta, CE. A paradigm shift for patient/family-centered care in intensive care units: Bring in the family. Crit Care Nurse. 2017;37(2):96-99.
Emergency Nursing Association. Clinical practice guideline: Family presence during invasive procedures and resuscitation. Updated 2012.
Powers KA. Barriers to family presence during resuscitation and strategies for improving nurses’ invitation to families. Appl Nurs Res. 2017;38:22-28.
ant7-Focus 0n CRITICAL CARE-618















2 Comments.
I am writing in response to the article entitled “Family presence during resuscitation in the intensive care unit” by Carolyn Bradley, Janet Parkosewich and Bertie Chuong, published in volume 13, issue 7 of American Nurse Today. As a recent ADN graduate and a first year Neurosurgical ICU nurse, I found this article extremely informative regarding the process of initiating family presence during resuscitation (FPDR) and how to become a change agent early in my career. FPDR is a controversial issue, not only for family members during these resuscitations, but also for the interdisciplinary staff assisting in the decision and process. This article accurately emphasizes the benefits of FPDR including reduction in family member’s anxiety, minimizing feelings of patient abandonment and the comfort provided knowing all efforts have been made to revive their loved ones. As noted by the authors, there are many driving and restraining forces that will either obstruct this change or expedite the outcome of implementation and success. One of the greatest hurdles initiating FPDR in an organization is changing the status quo and solidifying this policy into a unit’s culture. In my organization FPDR is in our policy, however I have found that lack of education provided to staff can be amongst one of the largest barriers in implementing FPDR effectively on our unit.
Kurt Lewin’s 3-step change model as explained in this article includes a step-by-step breakdown of how this can be implemented into an organization. One of the key pieces of information discussed is assembling an FPDR steering committee. This would need to be comprised of a multidisciplinary team who view FPDR as a benefit in patient center care. The controversy lies with the amount of education provided by an organization to promote this policy. It is interesting that as critical care nurses we are expected to promote and effectively implement FPDR on our unit, yet I have not been provided with any formal or informal education regarding why this policy exists in our organization. I’ve been in a classroom and clinical setting for the past 6 months as a new graduate critical care nurse and have learned abundant amounts of information regarding critical care and nursing. I am surprised that I have yet to be exposed or educated on this policy, especially since resuscitation is a common occurrence on all critical care units.
In an article entitled “Family Presence During Resuscitation: Impact of Online Learning on Nurses’ Perception and Self-confidence” published in July of 2016 in the American Journal of Critical Care, K.A. Powers and L. Candela performed a study that shows online learning is an effective tool when educating nurses on FPDR. One statistic that was astonishing in this study is out of the 72 critical care nurses in their sample size, only 29.7% worked in a facility or unit that had an FPDR policy and 41.9% actually had received any prior education on FPDR. One recommendation mentioned and could be very useful in implementing this education would be to add FPDR online learning in current ACLS certification renewal courses which increases its exposure to a majority of resuscitative care providers.
In conclusion, the authors provided a great resource of information on how to educate staff and implement FPDR policy in an organization. Although this policy has already been implemented in my unit, I find it to be less than effective as there is much room for improvement. After reading this article, I was inspired to center my critical care residency project, and my unit in-service, based on the lack of education that is provided by our healthcare system regarding FPDR. I believe that there is room to explore this topic and policy in my department while becoming the driving force to educate our unit as to why we are performing FPDR and how to perform it effectively. By utilizing the information provided in this article, I plan on being the change that will allow my organization to share a common vision in providing effective efforts in FPDR.
Sincerely,
Jamie Dupont, RN
I don’t know if it is policy but my son and I were permitted to remain in the ICU area during a resuscitation attempt on my wife. She wasn’t really conscious of our presence but it helped us in that we saw that everything possible was done .