A tool for patient safety and staff satisfaction.
By Idrialis Perez-Carter, MS, RN
Takeaways:
- Readers will be able to understand the purpose of staff rounding.
- Readers will identify one positive result that can result from having a successful rounding program.
- Readers will identify important measures required to have a successful rounding program
Geriatric psychiatric units are typically populated with patients who have a wide range of mental health diagnoses, including dementia, major depressive disorder, bipolar disorder, and schizophrenia. This diversity can be challenging for nursing staff as they attempt to meet the needs of both high-functioning and low-functioning patients. In addition, advanced age and complex medication regimens place many of these patients at risk for physical injury from falls.
 Just like acute care hospitals, psychiatric facilities must meet safety measures, such as fall prevention. In hospitals, hourly rounding (regular patient assessment) by staff has been linked to reduced patient fall rates and increased patient and staff satisfaction. However, to date, little has been published about rounding on inpatient geriatric psychiatric units.
Just like acute care hospitals, psychiatric facilities must meet safety measures, such as fall prevention. In hospitals, hourly rounding (regular patient assessment) by staff has been linked to reduced patient fall rates and increased patient and staff satisfaction. However, to date, little has been published about rounding on inpatient geriatric psychiatric units.
This article reviews a quality-improvement initiative conducted on the inpatient geriatric unit at a freestanding psychiatric hospital that included a rounding program.
Challenging patient population
The population of patients on this unit includes those with and without dementia. Those without dementia are usually defined as high functioning, and their ability to make their needs known and independently perform activities of daily living can result in staff overlooking their fall risk. Characteristics of patients with dementia include responsive behaviors—actions, words, or gestures that indicate something about their personal, social, or physical environment, sometimes related to stress or unmet needs. Despite the nursing staff’s conscientious attempts to identify and meet the needs of all their patients, they reported difficulty quickly addressing the needs of patients with dementia.
Planning the program
A workgroup made up of unit staff and administration, including the unit nurse manager, clinical assistant nurse manager, occupational therapists, and staff RNs and certified nursing assistants (CNAs) from day and evening shifts, developed a tool to encompass both the medical and psychiatric needs of the geriatric patients. They chose a 2-hour rounding interval by nurses rather than the more typical 1-hour interval because it would be less intrusive for patients with dementia who may require quiet and low stimulation.
Most geriatric psychiatric patients have medical diagnoses, so the workgroup included the four “Ps” (pain, personal needs, position, and possessions) in the rounding tool, with the addition of a fifth P for PO intake to ensure patient hydration and access to fluids. The workgroup chose the acronym ICARE for the rounding tool: Introduce, Comfort, Ask/Assess, Reassure/Reorient, and Environment. (See ICARE rounding tool.)
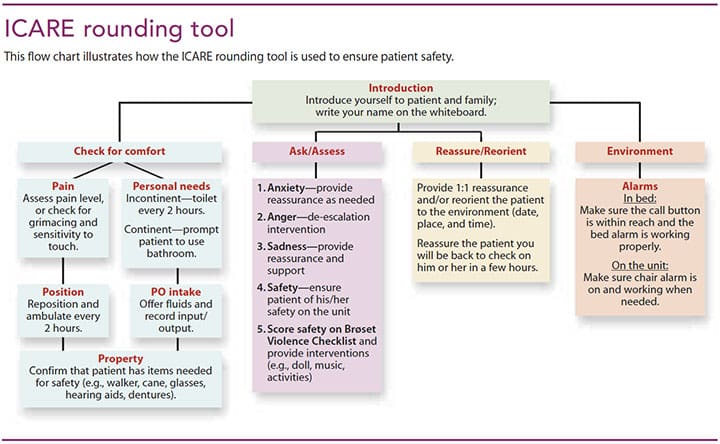
Introduce
Staff nurses introduce themselves to the patient and explain the rounding procedure. Education and understanding of the unit can decrease patient anxiety.
Comfort
Because patients with dementia may be unable to report their needs, the five Ps were incorporated into this step. Rounding staff check the patient’s comfort by assessing for pain (does the patient have pain), personal needs (does the patient have to use the bathroom), position (does the patient have to be repositioned or ambulated), possessions (are items such as hearing aids, glasses, and ambulatory aids within the patient’s reach), and PO intake (are fluids within reach).
Ask/assess
Nurses ask about and assess the patient’s symptoms of anxiety, anger, and depression. They also ask patients if they feel safe and may use a validated scale, such as the Brøset Violence Checklist to assess safety.
Reassure/reorient
Depending on the patient’s cognition level or need, rounding staff reassure the patient about his or her personal safety, provide orientation to time and place, validate concerns, and provide information about where family members are and when they’ll be visiting.
Environment
Safe organization of the physical environment, including the patient room and unit, plays a prime role in preventing patient falls. Rounding staff take the time to eliminate clutter, ensure adequate lighting, look for spills on the floor, and check that alarms are activated.
Rounding results
To date, results of the rounding program reveal a positive impact on staff satisfaction and patient safety, including a 70% reduction in falls per patient days during the first 3 months of the program compared to the previous 3 months. A survey distributed 3 months after the start of the program revealed increased staff satisfaction associated with nurses’ positive assessments of the quality of the healthcare they provide. One nurse commented, “Rounding is the best thing we have done on this unit. Even on the busiest day, I am able to get to all of my patients, and I feel good knowing that I met most of my patients’ needs.”
Proactive care
The positive outcomes—increased patient safety and improved staff satisfaction—of this quality-improvement initiative and accompanying ICARE tool are a catalyst for future studies of rounding models that may help nurses provide the proactive care geriatric patients with mental illnesses need and deserve.
Idrialis Perez-Carter is a nurse manager of the senior specialty program at Butler Hospital in Providence, Rhode Island.
Selected references
Almvik R, Woods P, Rasmussen K. Assessing risk for imminent violence in the elderly: The Brøset violence checklist. Int J Geriatr Psychiatry. 2007;22(9):862-7.
Dyck D, Theile T, Kebicz R, Klassen M, Erenberg C. Hourly rounding for falls prevention: A change initiative. Creat Nurs. 2013;19(3):153-8.
Hill E, Fauerbach LA. Fall and fall prevention in older adults. J Legal Nurse Consult. 2014;25(2):24-9.
Mawaka TP. Audit in improving dementia care on the inpatients wards. Br J Healthc Assist. 2012;6(4):177-81.
Moran J, Harris B, Ward-Miller S, Radosta M, Dorfman L, Espinosa L. Improving care on mental health wards with hourly nurse rounds. Nurs Manag (Harrow). 2011;18(1):22-6.
ant11-Rounding-1017a


















1 Comment.
A very good and information-rich article.