Providing the right care at the right time can enhance patients’ and families’ end-of-life experience.
Nurses frequently encounter patients who are changing their treatment goals to focus on comfort care, but they’re unable to return home because of symptom management concerns. At an academic medical center, an interprofessional team (including medical directors, nurse leaders/managers, clinical nurses, social workers, case managers, educators, and hospice staff) designed and implemented a floating hospice model to address these patients’ needs. The model was developed to offer hospice care to eligible patients throughout the hospital, including five intensive care units (ICUs), as a bridge until a hospice unit can be built.
Program development
The interprofessional team at our Magnet®-recognized hospital conducted a literature search to investigate how other organizations care for patients who want comfort care but can’t be discharged or transferred. The team noted various practices across the country and chose a “bring the hospice to the patient” model, which allows patients to stay within the hospital and continue care with the same nursing staff. The team then identified appropriate patients, defined caregiver roles, and developed workflows.
Key program features include:
- palliative care team becomes the attending provider
- patient enrolls in the hospice benefit
- hospital room is enhanced for patient and family comfort
- local hospice agency provides 24/7 onsite nursing support.
Palliative care team
The palliative care team has a consulting role in other areas of the hospital, but with this program, the team is responsible for patient management. This strategy promotes appropriate pain and symptom control.
Hospice benefit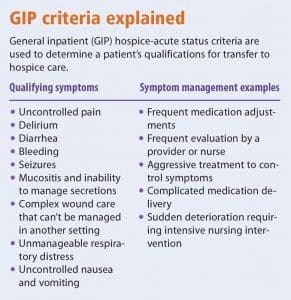
To qualify for the program, patients must be appropriate for general inpatient (GIP) criteria and must be
unstable for transfer to a residential hospice facility. GIP criteria are part of the Medicare hospice benefit, which allows an individual who has elected hospice care to receive general inpatient care for pain or acute or chronic symptom management that can’t be provided in other settings. (See GIP criteria explained.)
Room enhancement
Room enhancements include softer lighting, hanging artwork, music, aromatherapy, and an artistic movable screen for patient and family privacy. (See A room with a view…to end-of-life care.) These room enhancements might seem minor, but they make a difference to patients and families. We’ve received cards from families expressing how the room enhancements created a warm and comforting home-like setting.
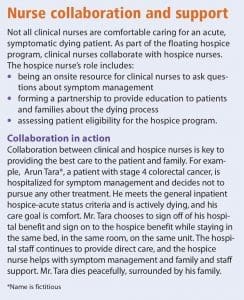
Nursing support
Clinical nurses are in a key position to provide end-of-life care with a hospice liaison as a resource. In the floating hospice, patients and their families receive nursing care from hospital nurses, while contracted hospice nurses focus on coordinating end-of-life education and supportive care. (See Nurse collaboration and support.)
Implementation
A staged implementation was planned in the medical ICU, the neurosciences ICU, one hematology-oncology unit, and one general medicine unit.
 Physician champions in these areas voiced interest in supporting their patients and families with a hospice care model. These units historically have patients with rapidly changing conditions that can result in a hospital death. With the physician champions and the hospice planning team, the program was successfully launched on January 12, 2015; it was rolled out to the remaining 20 inpatient units within 3 months.
Physician champions in these areas voiced interest in supporting their patients and families with a hospice care model. These units historically have patients with rapidly changing conditions that can result in a hospital death. With the physician champions and the hospice planning team, the program was successfully launched on January 12, 2015; it was rolled out to the remaining 20 inpatient units within 3 months.
Education
Education for all hospital staff was delivered via didactic presentations, tip sheets, and an intranet site. Education continues to be provided to new hires via a learning module and preceptor support. To make sure all staff were up-to-date on the hospice process and workflows, rolling education was provided to multiple departments. Members of the interprofessional team attended various departmental meetings to provide education about the new care model.
Challenges
The team encountered some initial challenges, including a knowledge deficit on the difference between hospice and palliative care and the work-flows in our electronic health record. To overcome these challenges, the palliative care attending providers presented at service line meetings, identified service line champions, developed patient case studies, and highlighted the benefits of this hospice model. In addition, the nurse educators attended staff meetings to provide face-to-face education, recruited unit-based hospice champions, and developed online education about the hospice program. The hospice nurses became the superusers for the electronic workflows, helping providers navigate the system to ensure complete and accurate documentation. Hospice nurses continue to collaborate with hospital staff by attending interprofessional rounds in the ICUs to assess patient eligibility and provide education.
Hospice patients aren’t moved in response to bed need. Instead, they’re assessed based on GIP criteria, and if it’s safe, they’re transferred to another setting for hospice care. For example, a patient in the ICU might be transferred to a medical/surgical unit that can provide hospice care so that another ICU patient can be admitted. Hospital leadership supports this protocol.
The hospice program caps the number of patients it admits. If the program is at capacity, an eligible patient remains an inpatient, and comfort and end-of-life orders are initiated. If possible, the patient is transferred to a hospice option outside of the hospital, but typically the patient’s clinical status prevents this.
Outcomes
From January 2015 to April 2019, the program served 650 patients with an average length of stay of 2.13 days. The program receives 41% of its referrals from the ICU. In a survey of inpatient nurses (response rate, 9.7%), 73% said they were satisfied or very satisfied with the hospice program. Some of the highlights from the survey show that most of the staff also value the program. One respondent said, “I feel that we really collaborate, and I enjoy the exchange of thoughts and ideas between us and the hospice nurses.” A satisfaction survey was developed for hospice families as well to capture their satisfaction with the program and the care they received. The families’ overall satisfaction rating was 96%.
Growing a program
Six months after starting the hospice program, the process improvement team explored options to grow it. Leadership support and momentum resulted in the ICU trigger tool, emergency department (ED)-to-hospice fast track projects, and increased referrals.
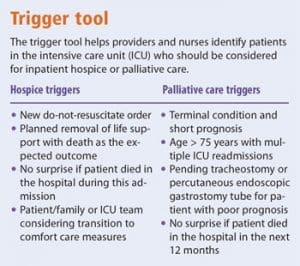 Trigger tool
Trigger tool
ED-to-hospice fast track
The goal of the ED-to-hospice fast track project was to find ways to identify eligible patients earlier, while they’re still in the ED, and then transition them quickly when the plan of care is comfort. A palliative care or hospice consult is provided in the ED, and the patient is transitioned to an inpatient bed when applicable. Patients and their loved ones are then provided care that meets their wishes and are able to avoid unwanted invasive medical testing or procedures.
Palliative care referrals
With the growth and awareness of the hospice program, referrals to palliative care increased, although not all were related to end-of-life or hospice care. As a result of education, providers, staff nurses, leaders, and the care management partners became more comfortable with their understanding of palliative care, which has led to more interprofessional team discussions about how to incorporate this care throughout the hospital and more consults.
Enhancing end-of-life care
This inpatient hospice model enhances the patient and family experience at the end of life. Development, education, and support for clinical nurses is an ongoing process, and the model has a positive impact on how nurses perceive their role during the dying process. Floating hospice programs are feasible in the hospital setting, but preparing for potential challenges will enhance the likelihood of successful implementation.
Colleen McCracken is a staff RN/educator in hematology/oncology/palliative care at Froedtert Hospital in Milwaukee, Wisconsin. Katherine Walczak is a palliative care clinic nurse at Community Hospital Division in Menomonee Falls, Wisconsin.



















4 Comments.
As I type one of my oldest and dearest friends is in Hospice in Houston, Texas. His wife tells me it is one of the pleasant and relaxing places for her at this time, it will be a good memory for her after he passes.
Your blog is very useful and provides tremendous facts. Keep up the good work.
As a hospice nurse, I appreciate this innovative approach on multiple fronts.
This offers the opportunity for the patient and family to engage sooner with both Palliative and Hospice care providers, and get onto the Hospice Benefit. Since many patients tell us they wish to die at home, this allows the patient the chance to be in a “home-like” environment where they can receive an appropriate level of care and stabilize symptoms before returning home. I can see this serving as an excellent model of care whether the hospital has an in-patient hospice unit, or whether there is referral to a community based hospice.
I serve on the board of our local chapter (San Francisco Bay Area) of the Hospice and Palliative Nurses Association (HPNA) and plan to share your article with our membership.
This must be one of the most challenging duties. In the past few years, I’ve tended to both a best friend and my own Mother in Hospice, I can never thank the nurses enough for what they did to support Me while these two dear people transitioned.