Timely assessment and prevention improve patient outcomes.
Takeaways:
- Nurses play a vital role in the promotion of healthy patient skin.
- Incontinence-associated dermatitis (IAD) is a common skin injury resulting from the excessive exposure of skin to urine and stool, causing patient pain and discomfort.
- Nursing assessment of risk factors and the implementation of a structured skin care regimen can reduce the incidence of IAD.
- Timely identification of skin injury and implementation of appropriate treatment can limit the extent of IAD skin injury.
By Kathleen Francis, DNP, FNP-BC, CWOCN
 When your patient’s skin is repeatedly exposed to moisture from urine and feces, he or she is at risk for incontinence-associated dermatitis (IAD), which can result in discomfort, loss of independence, disruption in daily activities, embarrassment, and a reduced quality of life.
When your patient’s skin is repeatedly exposed to moisture from urine and feces, he or she is at risk for incontinence-associated dermatitis (IAD), which can result in discomfort, loss of independence, disruption in daily activities, embarrassment, and a reduced quality of life.
IAD affects the perianal area, perineum, buttocks, and thighs; it’s most severe when the patient experiences frequent episodes of incontinence and exposure to liquid fecal effluent. (See How skin functions: A refresher.) Patients with IAD frequently report pain, burning, itching, and tingling in the affected areas.
IAD is common, but prevalence varies depending on the healthcare setting, with rates ranging between 3.5% and 42%. And as hospitals reduce the number of indwelling catheter days to prevent catheter-
associated urinary tract infections, IAD incidence rates in acute care settings have risen.
The National Pressure Ulcer Advisory Panel guidelines suggest that moisture-associated skin damage, such as IAD, can increase the risk of pressure injury (PI). Because PI rates are nationally reported quality indicators for nursing care, IAD assessment, prevention, and management are essential to any facility’s skin care program.
Assessment
 Establishing the presence of incontinence is essential to identifying patients at risk for IAD. Patients may be reluctant to tell you about their incontinence if you don’t ask, so your initial history and physical exam should include questions about it, including type (urinary or fecal) and frequency. Ask the patient or caregiver about toileting and bathing routines and if there have been any “accidents.”
Establishing the presence of incontinence is essential to identifying patients at risk for IAD. Patients may be reluctant to tell you about their incontinence if you don’t ask, so your initial history and physical exam should include questions about it, including type (urinary or fecal) and frequency. Ask the patient or caregiver about toileting and bathing routines and if there have been any “accidents.”
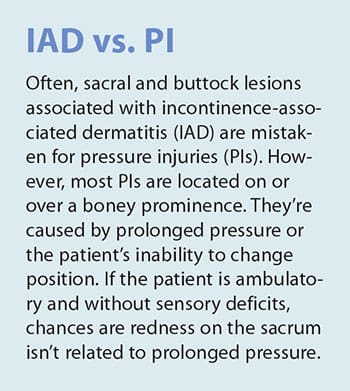
Inspect the patient’s skin, including perigenital skin, noting color, turgor, moisture, temperature, and the presence or absence of skin injuries. Adequate lighting will help you see any subtle changes in skin color. (See IAD vs PI.) Repeat skin assessments as needed. Patients who are incontinent should be assessed more frequently because they’re at increased risk for IAD.
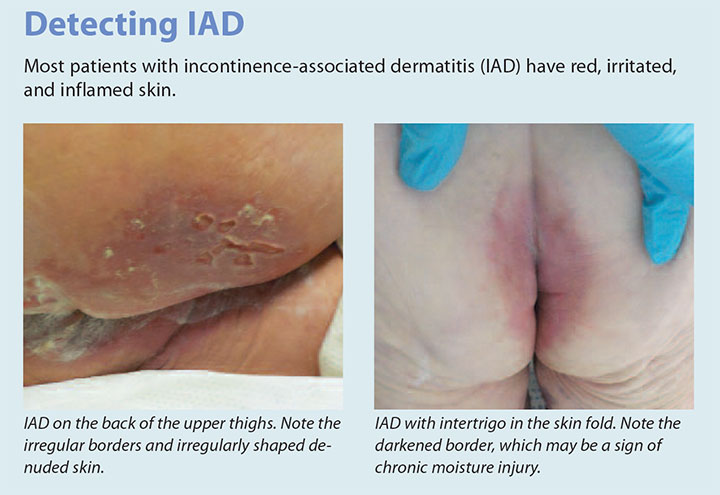
The classic presentation of IAD is moist, reddened skin and inflammation. (See Detecting IAD.) You may see diffuse epithelial edema and irregular borders with or without weeping and blistering. Satellite lesions are typically caused by secondary cutaneous candidiasis, which is associated with more severe cases of IAD. In patients with darker skin tones, redness may be more subtle and may appear as a discoloration when compared to the surrounding skin. Most patients will report a burning sensation with pain and pruritus in the area of discoloration.
Prevention
Identifying the cause of incontinence can help determine appropriate interventions to limit episodes and protect the skin. For example, the patient with functional incontinence can identify the need to void or defecate but can’t physically get to the bathroom without assistance. Implementing a plan to assist the patient can limit the episodes of incontinence. For a patient who has urinary incontinence caused by neurogenic bladder from a spinal cord injury, implementing a program with clean intermittent catheterization will limit episodes of urinary incontinence and prevent nephritis. In both of these examples, placing the patient in an incontinence brief won’t limit the episodes of incontinence and will expose the skin to unnecessary moisture.
Toileting
Structured toileting programs, when appropriate, can significantly reduce the patient’s exposure to moisture. External devices to contain urinary or fecal incontinence, such as pouches and condom catheters, can be used based on individual patient needs. Indwelling urinary or fecal catheters should be an option of last resort because they make the patient more vulnerable to infection.
Absorbent products
Using absorbent products in combination with frequent garment changing will help keep skin dry and prevent fungal dermatitis. Absorbent incontinence products, such as pads or briefs worn by the patient and pads placed on the bed or chair, quickly wick moisture away from the skin to reduce IAD risk.
To avoid fungal dermatitis that can occur from occlusion of the perineal area in bed-bound patients in the acute care setting, body-worn briefs should be limited to ambulatory patients or those who use a wheelchair or are chair-bound. Absorbent incontinence pads allow for effective dissipation of moisture from the perineal area in bed-bound patients.
Patient preference and need also may play a role in product choice. For example, some hospitalized patients may prefer body-worn briefs to maintain their dignity. Although many absorbent products provide improved fluid handling and incorporate a breathable outer liner, the benefit of generalized use in acute care hasn’t been established.
Skin care
Skin care to prevent IAD includes three steps.
- Gently clean the skin with a soft cloth and a no-rinse cleansing product that contains surfactants to loosen irritants. Avoid products that require rinsing and drying the skin with a towel. Choose a soft cloth to limit friction damage to the area and a cleanser with a pH range consistent with the skin’s acid mantle.
- After cleaning the skin, apply moisturizer to replenish intracellular lipids and maintain the skin’s moisture barrier function.
- Apply a moisture barrier ointment to protect the skin from effluent. These ointments may contain petroleum, dimethicone, or zinc oxide.
Another option is an all-in-one soft cloth that contains a cleanser, moisturizer, and barrier. Some evidence supports the use of all-in-one products because they’re easier to use and ensure all three steps are routinely implemented.
Management
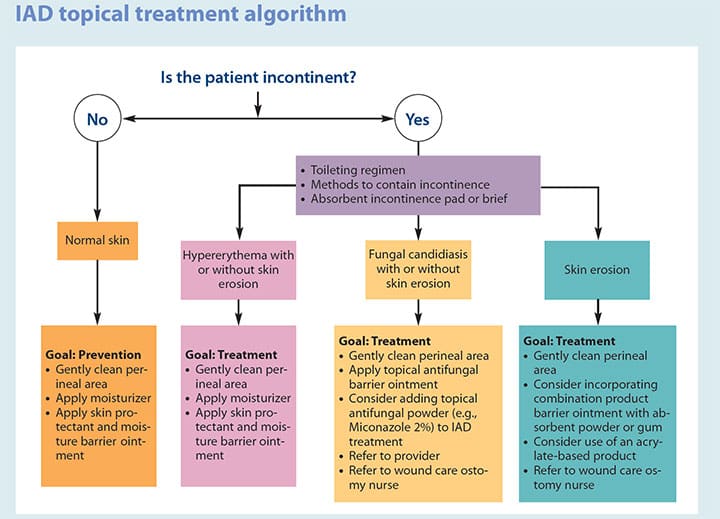
In addition to prevention and skin care, other treatments include antifungal barrier ointments or powders for treating candidiasis or cutaneous fungal rash. Reserve antifungal therapies for patients with fungal dermatitis; don’t use them for uncomplicated IAD.
Topical steroids and antimicrobials should not be used regularly. Topical steroids can mute the symptoms of IAD and fungal dermatitis, but they don’t treat the underlying cause. Reserve their use for dermatologic skin conditions, such as atopic dermatitis. Antimicrobials, which can reduce healthy skin flora and increase the risk of dermatologic infection, are appropriate only if the patient presents with a skin infection. For severe cases of fungal incontinence dermatitis, a combination product, such as nystatin-triamcinolone, can be considered.
For complicated cases of IAD that don’t respond to treatment within 2 weeks, refer the patient to a wound specialist, such as a wound ostomy continence nurse or a dermatologist. (See IAD topical treatment algorithm.)
Timely care
Nurses play an important role in promoting healthy skin and reducing injury. Skin care of patients with IAD requires timely assessment, prevention, and management, as well as knowledge of the interventions and products that can help ensure skin integrity.
Kathleen Francis is the wound ostomy continence team coordinator at Maimonides Medical Center in Brooklyn, New York.
Selected references
Corcoran E, Woodward S. Incontinence-associated dermatitis in the elderly: Treatment options. Br J Nurs. 2013;22(8):450-7.
Doughty DB, McNichol LL. General concepts related to skin and soft tissue injury caused by mechanical factors. In Wound, Ostomy and Continence Nurses Society Core Curriculum: Wound Management. Philadelphia, PA: Wolters Kluwer; 2016; 273-9.
Doughty D, Junkin J, Kurz P, et. al. Incontinence-associated dermatitis: Consensus statements, evidence-based guidelines for preventions and treatment, and current challenges. J Wound Ostomy Continence Nurs. 2012;39(3):303-15.
Gray M, Beeckman D, Bliss DZ, et al. Incontinence-associated dermatitis: A comprehensive review and update. J Wound Ostomy Continence Nurs. 2012;39(1):61-74.
Mufti A, Ayello EA, Sibbald RG. Anatomy and physiology of the skin. In Doughty DB, McNichol LL, Eds. Wound, Ostomy and Continence Nurses Society™ Core Curriculum: Wound Management. Philadelphia, PA: Wolters Kluwer; 2016; 3-23.
Nazarko L. Use of continence pads to manage urinary incontinence in older people. Br J Community Nurs. 2015;20(8):378, 380, 382-4.
Rippon M, Colegrave M, Ousey K. Incontinence-associated dermatitis: Reducing adverse events. Br J Nurs. 2016;25(18):1016-21.
Woo KY, Beekman D, Chakravarthy D. Management of moisture-associated skin damage: A scoping review. Adv Skin Wound Care. 2017;30(11):494-501.
ant1-Focus 0n Wound Care-1218