Lawrence Jeffries, age 78, is admitted to the hospital for an arthroplasty of the left hip. A retired roofer, he lives with his wife and son in a two-story home. He has a history of arthritis and type 2 diabetes, which has been controlled with tolazamide 100 mg daily. On the second post-op day, his nurse, Jessica, notes that he slept most of the morning and fell asleep after physical therapy in the afternoon.
When his wife visits at lunch time, she tells Jessica her husband is picking at the bedding and complaining of feeling cold. Jessica has the nursing assistant give him a warm blanket. Later in the afternoon, Mr. Jeffries puts on his call light. When you respond, he states, “I can’t figure out how to get my TV on.” You remind him you explained how to use the TV remote yesterday, and ask if he has trouble remembering things. He states he didn’t have trouble until he came to the hospital. He complains of pain in his left hip and says he doesn’t think he has had any pain medication today. However, you know he received morphine 4 hours ago. He asks again about getting his TV working.
When Mr. Jeffries’ son visits later, you question him about his father’s memory. He confirms his father had no trouble with his memory before.
In a scenario like this, the nurse should ask herself if delirium could be causing the patient’s signs and symptoms. A medical emergency that occurs in up to 56% of hospitalized older adults, delirium is marked by sudden onset of confusion (over a few hours or days), inattention, illogical thinking or incoherent speech, altered sleep-wake cycle, and changes in psychomotor behaviors. Signs and symptoms fluctuate over time, with the patient seeming to float in and out of confusion. Delirium manifestations may go unrecognized in hospital patients because most healthcare professionals aren’t familiar with the patient’s usual behaviors or baseline cognitive status.
Consequences of delirium for older adults may include increased mortality, functional decline, nursing home placement, and decreased quality of life. Longer duration of delirium is linked to poorer health outcomes among older adults, underscoring the need for early detection and intervention.
Delirium also exacts a high economic price. Estimated annual U.S. healthcare expenditures range from $143 to $152 billion, with increased hospital stays contributing heavily.
Delirium can be frightening for both patients and for family members who observe it in their loved ones. As a nurse, you can play a key role in identifying risk factors, detecting symptoms early, implementing nonpharmacologic interventions promptly, and educating family members about the disorder.
Who’s at risk
Older adults, particularly those over age 70, are more likely than younger adults to develop delirium when hospitalized. Other factors that place older adults at risk include dementia, alcohol abuse, impaired physical function, sensory impairment, sleep deprivation, poor oxygenation, uncontrolled pain, and taking four or more medications. Mr. Jeffries in our case scenario has some of these risk factors.
Causes and types of delirium
Factors that can cause or contribute to delirium include:
- dehydration
- infection
- drug toxicity
- polypharmacy
- adverse drug reactions
- immobility (including restraint use)
- severe pain
- urinary retention
- metabolic or electrolyte imbalances. In a patient with dehydration, the serum sodium level may rise, causing increased blood pressure.
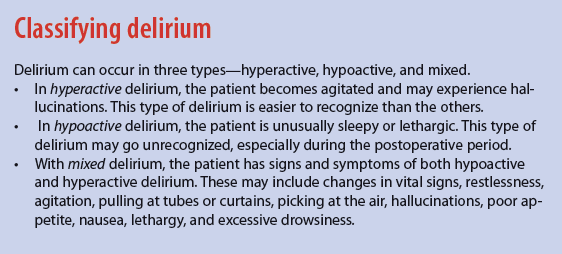
Delirium occurs in three types. (See Classifying delirium.)
Signs and symptoms
Depending on the type of delirium, signs and symptoms may include:
- agitation
- hallucinations
- sleepiness
- lethargy.
Assessing for delirium
To detect a change in the patient’s cognition, you need to know his or her baseline status. Acute delirium poses a challenge to nurses who didn’t meet the patient before admission or haven’t cared for him or her on consecutive days. To help determine if a sudden cognitive change has occurred, question family members about the patient’s usual cognitive status.
Using a standardized assessment tool, evaluate the patient for delirium signs and symptoms during each shift or when you note cognitive changes. Several valid and reliable standardized tools exist for delirium screening. The Confusion Assessment Method (CAM) is an evidence-based tool you can use to identify delirium quickly, easily, and correctly. It’s the most widely used tool in published studies, with extensive reports on its validity and reliability in older adults.
Separate versions of CAM have been developed for use in clinical practice. The CAM short form (CAM SF) takes 5 minutes to complete. The 3D-CAM takes only 3 minutes and is recommended when a quick assessment is needed. Both forms assess for key characteristics of delirium, including sudden onset, fluctuating course, inattention, disorganized thinking, and altered levels of consciousness. Both CAM forms and their instructions are available from Hospital Elder Life Program for Prevention of Delirium at http://www.hospitalelderlifeprogram.org/delirium-instruments/confusion-assessment-method-long-cam.
Sudden onset and inattention, plus either disorganized thinking or an altered level of consciousness, indicate a positive screen on CAM. Patients with a positive screen require further evaluation by a physician or an advanced practice nurse to identify the cause and initiate appropriate interventions.
Nurse Jessica uses CAM to assess Mr. Jeffries for delirium, based on her observation of excessive drowsiness, his wife’s report of him picking at his bedding, and his complaint of pain despite his medication. The test shows his attention span is limited. These results indicate a positive screen for delirium, so she immediately contacts the physician to ensure a more thorough evaluation.
Nonpharmacologic interventions
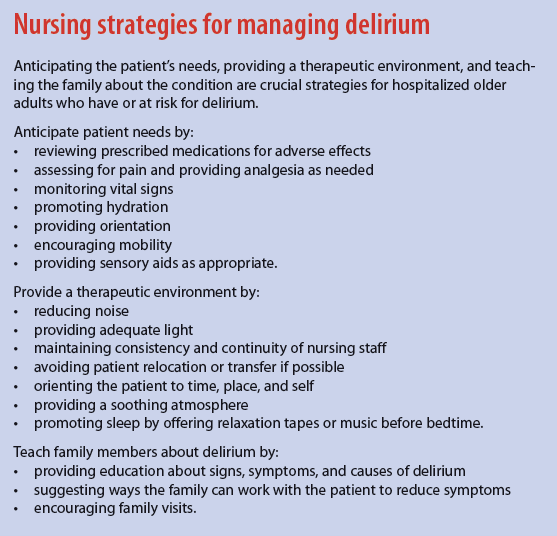
Delirium may be reversible if detected and treated early. In some cases, it can be prevented by identifying risk factors and initiating evidence-based nonpharmacologic measures. These measures include:
- providing a therapeutic environment
- orienting the patient frequently
- anticipating the patient’s needs
- ensuring that hearing aids and eyeglasses are available for patients who use them
- observing the patient’s response to medications
- checking laboratory tests.
To provide a therapeutic environment, orient the patient to time, place, and self. Minimize noise and ensure appropriate lighting to reduce environmental stimuli and promote rest. (See Nursing strategies for managing delirium.)
Anticipating the patient’s needs requires astute assessment and direct patient care. Assess the patient’s cognitive status, vital signs, medications, and pain level. Monitor vital signs to help identify complications, such as infection and dehydration. For example, low blood pressure may suggest dehydration, irregular breathing may indicate hypoxia, and an elevated temperature might reflect dehydration or infection.
Review prescribed medications, as some drugs may cause adverse effects that increase delirium risk. Assess for pain regularly; severe pain can contribute to delirium. As needed and ordered, administer analgesics to promote effective pain management.
Other direct-care strategies include orienting the patient to time, place, and self and keeping a clock and calendar in the room. In addition, be sure to use clear, concise communication. For instance, tell the patient what you’re going to do and why, speaking in short sentences because the patient might have a short attention span. Encourage mobility to the extent allowed, and ensure adequate food and fluid intake to prevent dehydration. If the patient uses dentures or sensory aids, such as a hearing aid or eyeglasses, keep these available and clean.
Educating family members
Teaching the patient’s family about delirium can aid its detection and management. When a family member reports a loved one isn’t acting like himself or herself or “just isn’t acting right,” take this information seriously.
Remember—delirium signs and symptoms can elicit fear and anxiety in family members, who typically lack knowledge about the disorder, its causes, and how to help their loved one. To reduce their anxiety, educate them about delirium, potential causes, and manifestations. Enlist the family’s help to promote early recognition of the disorder. Encourage them to visit the patient and bring diversional activities he or she enjoys, such as newspapers, magazines, or puzzles. Urge them to provide reassurance to their loved one and engage the patient in conversation about current events. To help promote a safe environment, ask family members to contact the nurse if their loved one tries to get out of bed without assistance, pulls at tubes or dressings, or needs pain medication.
The nurse’s vital role
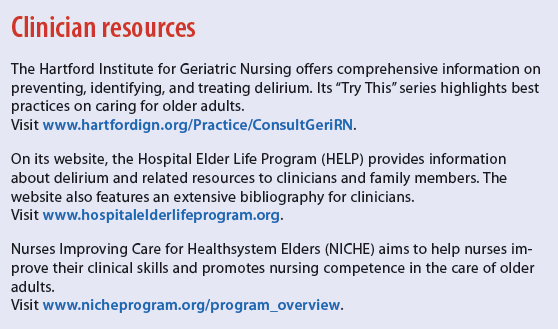
You can play a vital role in detecting delirium early and promoting comfort for older adults with this condition. To provide evidence-based care, assess and anticipate the patient’s needs. Teach family members about delirium symptoms and causes, and suggest ways for them to promote comfort during their loved one’s stay. (See Clinician resources.)
After learning of Mr. Jeffries’ positive delirium screen, the attending physician replaces morphine with tramadol 50 mg P.O. every 4 to 6 hours. Jessica explains to the patient’s family that delirium symptoms can reflect an adverse drug reaction and the physician thought morphine might have caused Mr. Jeffries’ symptoms. She encourages them to alert her if they notice that he seems confused. She also teaches them that tramadol shouldn’t be stopped abruptly and that Mr. Jeffries should avoid alcohol when taking the medication.
Two days after discontinuing morphine, Mr. Jeffries’ delirium resolves. On the fifth day after surgery, he’s transferred to inpatient rehabilitation.
Margaret J. Bull is a professor at Marquette University College of Nursing in Milwaukee, Wisconsin. Names in the clinical scenario are fictitious.
Selected references
Bélanger L, Ducharme F. Patients’ and nurses’ experiences of delirium: a review of qualitative studies. Nurs Crit Care. 2011; 16(6):303-15.
Bull MJ, Boaz L, Sjostedt J. Family caregivers’ knowledge of delirium and preferred modalities for receipt of information. J Appl Gerontol. 2014 Jun 18.
Dasgupta M, Brymer C. Prognosis of delirium in hospitalized elderly: worse than we thought. Int J Geriatr Psychiatry. 2014;29(5):497-505.
DeCrane SK, Sands L, Ashland M, et al. Factors associated with recovery from early postoperative delirium. J PeriAnesth Nurs. 2011;26(4):231-41.
Hshieh T, Yue J, Oh E, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA. 2015;175(4):512-20.
Leslie DL, Inouye SK. The importance of delirium: economic and societal costs. J Am Geriatr Soc. 2011;59 Suppl 2:S241-3.
Martinez FT, Tobar C, Beddings CI, et al. Preventing delirium in an acute hospital using a non-pharmacological intervention. Age Ageing. 2012;41(5):629-34.
Otani H, Morita T, Satsuki U, et al. Usefulness of the leaflet-based intervention for family members of terminally ill cancer patients with delirium. J Palliat Med. 2013;16(4):419-22.
Rosenbloom-Brunton DA, Henneman EA, Inouye SK. Feasibility of family participation in a delirium prevention program for hospitalized older adults. J Gerontol Nurs. 2010;36(9):22-33.
Rubin FH, Neal K, Fenlon K, et al. Sustainability and scalability of the hospital elder life program at a community hospital. J Am Geriatr Soc. 2011;59(2):359-65.
Saczynski JS, Marcantonio ER, Quach L, et al. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012;367(1):30-9.
Sykes PK. Prevention and management of postoperative delirium among older patients on an orthopedic surgical unit: a best practice implementation project. J Nurs Care Qual. 2012;27(2):146-53.
Tullmann DF, Fletcher K, Foreman MD. Geriatric nursing protocol: Delirium: Prevention, early recognition, and treatment. In: Boltz M, Capezuti E, Fulmer TT, et al, eds. Evidence-Based Geriatric Nursing Protocols for Best Practice. 4th ed. New York, NY: Springer Publishing Co.; 2011. http://consultgerirn.org/topics/delirium/want_to_know_more