Abuse in the workplace should never be tolerated. But, of course, it is. Nurses frequently experience abuse and harassment where they practice, learn, teach, research, and lead. Unfortunately, many victims don’t report abuse. And for those who do report it, the reward may be retaliation rather than an effective response.
Defining workplace abuse
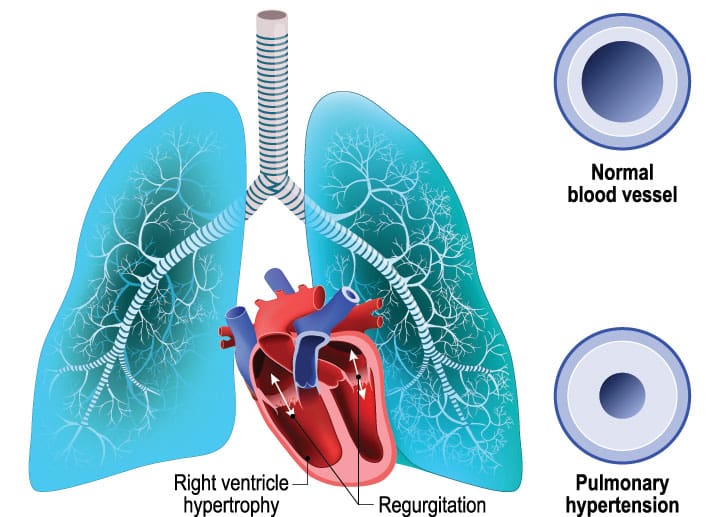
Abuse is any behavior that humiliates, degrades, or disrespects another, including intimidating behaviors, such as using condescending language, exploding in angry outbursts, using threatening body language, and making physical contact. The emotional impact of abuse demoralizes victims and can leave them feeling personally and professionally attacked or devalued. Victims also suffer physical consequences, such as loss of sleep, anxiety attacks, hypertension, and weight fluctuations.
We may tend to think of physicians as the prime perpetrators of abuse against nurses. But we now know that abuse in the workplace can also come from co-workers, supervisors, and even patients. Factors contributing to workplace violence include stress, poor staffing levels, long working hours, improper training of personnel, and power and control issues.
After experiencing abuse, many nurses feel powerless to do anything about it. Some believe no one really cares, so most acts of abuse and harassment probably aren’t reported. And this tolerance probably escalates the problem. Interestingly, research shows that inexperienced nurses are more likely to report workplace abuse than experienced nurses, who are more likely to believe that policies and procedures for workplace abuse and harassment are ineffective.
Fixing the problem
Finding ways to create workplace environments that discourage abuse and harassment of nurses is long overdue. Because of the worsening national nursing shortage, many professional organizations have examined factors that lead to job satisfaction and dissatisfaction among nurses. In 2004, the American Association of Critical-Care Nurses (AACN) identified verbal abuse and disrespectful behavior from co-workers, peers, and colleagues as serious nursing concerns.
As a recent study on workplace violence indicates, abuse in the workplace will continue, unless programs that establish, enforce, and measure zero-tolerance policies are put into action. The Nursing Organizations Alliance established principles and elements of a healthful practice and work environment in 2004. The American Nurses Association and several other nursing organizations have endorsed these principles and elements.
In 2005, the American Organization of Nurse Executives set as a strategic goal encouraging research that promotes positive practice environments. Other professional nursing organizations, such as AACN and the National Association of School Nurses, have established principles for supporting healthy work environments, where deferential communication and behavior, trust, shared decision making, and a culture of accountability are endorsed.
Handling abuse
As nurses, we must continue to develop programs that discourage abuse and harassment, and we must implement and support them in the workplace. Familiarize yourself with your organization’s policies and procedures against abuse, harassment, and hostile work environments. You should also be familiar with the mechanisms for reporting abuse and the protections afforded nurses after reporting it. Remember, organizations have a responsibility to ensure that nurses feel safe reporting incidents of abuse and harassment.
When confronted with abuse, try these empowering interventions:
• Remain calm.
• Speak calmly in a low voice.
• If you can’t control the situation in a timely way, call for help.
• Maintain a nonthreatening body posture, keeping your arms loose and at your side. Crossing your arms sends the message that you are angry and a potential threat to the perpetrator.
• Move to the vicinity of an exit, such as a door or the stairs. If possible, don’t allow the perpetrator to block your exit.
• Excuse yourself from a physically threatening situation and notify security, your supervisor, clinical instructor, and preceptor immediately.
Report abuse immediately to supervisors and the human resources department. The matter should then be elevated to more senior leadership in the organization until the problem is appropriately addressed. Be sure to keep detailed documentation on the abuse. Written reports should include the date and time of the incident, the names and titles of those involved, the nature of the abusive behavior, the names of witnesses, the actions taken, and the results of the actions taken.
You also need to find a way to let go of the anger the episode triggered. Research shows that holding on to bad feelings toward the perpetrator only prolongs recovery and delays resolution. Consulting a mental-health advanced practice nurse can help both victims and witnesses.
Costs of abuse
Abuse and hostility significantly decrease morale, diminish job satisfaction, and influence where nurses practice, learn, teach, research, and lead. If such behavior is allowed to continue, the costs to healthcare organizations and ultimately the nursing profession will be enormous. A conservative cost estimate of violence in the workplace is $4.3 billion annually or about $250,000 per incident.
Abuse and harassment in the healthcare setting have become a significant reason for lost time from work, increased absenteeism, lost productivity, and even occupational injury. This list doesn’t even begin to take into consideration the hidden expenses from the emotional pain victims, witnesses, and families suffer, such as anxiety, depression, and feelings of isolation.
Improving healthcare environments for nurses will improve patient outcomes as well as nurse recruitment and retention. Without safe, healthy work environments for nurses, quality healthcare delivery may decline. To avoid these costs, organizations and nurses must address the problems that put nurses in harm’s way.
Selected references
Cardillo D. End workplace abuse. dcardillo.com/articles/workplaceabuse.html. Accessed April 23, 2008.
Greene J. The medical workplace: no abuse zone. Hosp Health Netw. 2002;6:26-28.
International Council of Nurses. Guidelines on coping with violence in the workplace. http://www.icn.ch/images/stories/documents/publications/guidelines/guideline_violence.pdf. Accessed April 23, 2008.
Nursing Organizations Alliance. Principles & elements of a healthful practice/work environment. www.nursing-alliance.org/. Accessed April 23, 2008.
Occupational Safety and Health Administration. Workplace violence. www.osha.gov/SLTC/workplaceviolence. Accessed April 23, 2008.
Visit www.AmericanNurseToday.com/journal for a complete list of selected references.
John S. Murray, Colonel, United States Air Force, is Director of Education, Training & Research for Joint Task Force National Capital Region Medical in Bethesda, Md. and President of the Federal Nurses Association. The views expressed in this article are those of the author and do not reflect the official policy or position of the United States Air Force, Department of Defense, or the federal government.
















1 Comment.
Thank you for this article