Education can help nursing staff gain control and improve patient safety.
Takeaways:
- A standardized unit-based education program increases nurse awareness of clinical alarm fatigue.
- Nurses become desensitized to noise created by audible nonactionable alarms.
By Sharon H. Allan, DNP, ACNS-BC, CCRC
Someone with an outside perspective may be surprised by the noise and chaos of an intensive care unit (ICU), where alarms go off repeatedly. But nurses and others who work in that environment every day too often think the chaos is normal, when in fact it’s creating distraction and jeopardizing patients.
Alarms have a long history of compromising patient safety, and recent studies demonstrate the negative consequences alarms have on families and nurses as well. To highlight the importance of this issue, for the fifth year in a row, reduction of clinical alarm harm is a Joint Commission National Patient Safety Goal.
 To address this problem, a team of interdisciplinary professionals—including human factors engineers, clinical engineers, a unit-based nurse manager, a unit medical director, a unit-based clinical nurse specialist, a central nursing clinical nurse specialist, and expert bedside nurses—at a large academic medical institution launched a quality improvement (QI) project to look into the effects of alarm fatigue and strategies to reduce the number of nonactionable alarms.
To address this problem, a team of interdisciplinary professionals—including human factors engineers, clinical engineers, a unit-based nurse manager, a unit medical director, a unit-based clinical nurse specialist, a central nursing clinical nurse specialist, and expert bedside nurses—at a large academic medical institution launched a quality improvement (QI) project to look into the effects of alarm fatigue and strategies to reduce the number of nonactionable alarms.
Identifying the problem
ICUs are high-intensity environments that require clinical staff vigilance, but nonactionable nuisance alarms pull them away from high-priority tasks, creating staff dissatisfaction and a patient safety hazard. When the QI project team reviewed clinical alarm data, they discovered that alarm fatigue was institution-wide. During a patient safety meeting with ICU nurses, several of them indicated that one of the alerts being discussed was “message only.” However, it was one of several auditory alarms that they heard several times a day. This is a prime example of how too much alarm noise created by nonactionable auditory alerts leads to alarm fatigue. Your brain isn’t able to process all the sensory input, so sounds that aren’t the result of a change in a patient’s physiologic state aren’t thoroughly processed, which can lead to missing an actionable alert.
The team conducted a literature review, which revealed that educational interventions targeting staff awareness of alarm fatigue may improve compliance with alarm management strategies.
Gathering data
The QI team wanted to measure nurse awareness and perception of alarm burden before and after an education intervention aimed at increasing nurse awareness. The team chose the National Clinical Alarm Survey, developed by the Healthcare Technology Foundation (HTF), to establish baseline perception and awareness. The HTF survey tool has been used to provide data on nurse awareness of alarm fatigue and the stress related to excessive clinical monitor alarms. The survey link was emailed to all of the nurses working in the ICU. The body of the email provided an overview of the project; when nurses opened the link to take the survey, they gave their consent to participate in the project.
Intervention through education
After completing the pre-intervention survey, nurses participated in intense education sessions for 8 weeks. The varied sessions included staff participation in developing education posters with weekly unit-specific alarm data, reading and discussing articles on the negative impact of alarm fatigue, and exploring best practice alarm management strategies, such as alarm customization.
The posters were displayed in the staff team room. At weekly multidisciplinary comprehensive unit-based safety program meetings, an overview of the QI project was shared, along with education on the number of nonactionable alarms in the ICU and best practices to reduce alarm burden. Members of the QI team also conducted weekly one-on-one sessions with bedside nurses to measure real-time compliance with alarm customization.
Perception vs. reality
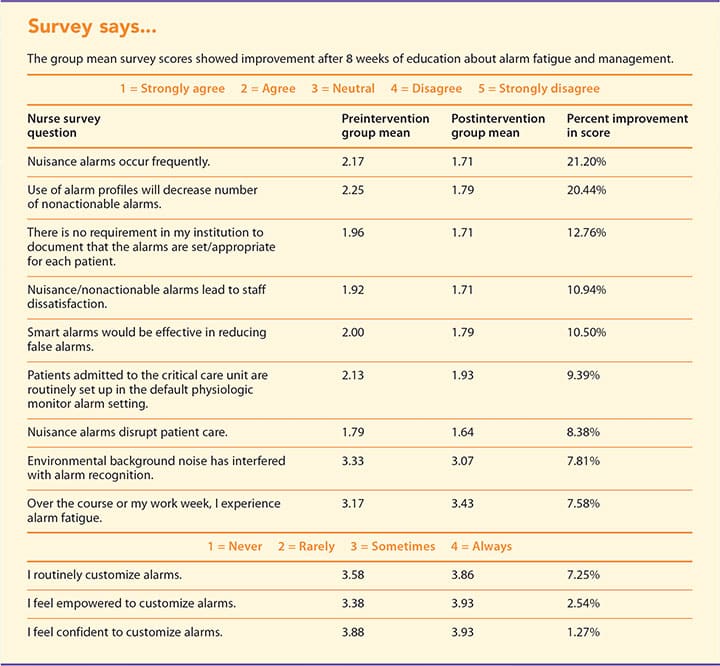
Pre- and postintervention nurse awareness survey results were compared to see if staff compliance and confidence with customized alarm settings improved. The goal was to achieve a 20% improvement in survey results specific to questions that measure nurse awareness and perception of alarm fatigue. A total of 38% (n=23) of the nursing staff participated in the preintervention survey and 21% of the nurses (n=13) volunteered to participate in the postintervention survey. Descriptive statistics were run to compare pre- and postintervention group means and determine if improved scores were clinically significant. (See Survey says….) Nurse knowledge of alarm fatigue, customization of alarm settings, and awareness of nuisance alarms improved. The practice change showed improvement in all areas of the survey.
The preintervention survey data reflected the nurses’ perception that they were knowledgeable about alarm fatigue and alarm customization, and that they demonstrated high compliance with alarm management strategies aimed at reducing alarm burden. However, during education sessions, the QI team found that many of the nurses didn’t have the knowledge or confidence to customize alarms, and that they weren’t able to define or describe alarm fatigue.
What we learned
This QI project resulted in overall clinical improvement in nurse awareness and knowledge of alarm fatigue and improvement in compliance with best practice changes to reduce alarm burden. The small sample size, time constraints, and length of the survey limited the number of nurses who could participate.
Improving staff compliance with strategies to reduce alarm burden may benefit from preintervention one-on-one sessions to evaluate nurses’ baseline practical skills on the use of best practice alarm-reduction strategies. The intervention also might benefit from a tool that assesses nurses’ personal awareness and perception and compares those results with their actual knowledge and understanding.
The QI team will disseminate the nursing implications of this project as recommendations for future standards of care to help improve nursing practice and alarm management.
Take control
When you’re in the thick of a busy, noisy ICU, you might not realize the impact of multiple alarms vying for your attention. Education about the ramifications of nurse fatigue and the benefits of alarm-reduction strategies may help you and your colleagues gain control of the situation, improve your work environment, and ensure patient safety.
Sharon H. Allan is a clinical nurse specialist appointed program track coordinator, acute and chronic care, at The Johns Hopkins University School of Nursing, Baltimore, Maryland.
Selected references
Allan SH, Doyle PA, Sapirstein A, Cvach M. Data-driven implementation of alarm reduction interventions in a cardiovascular surgical ICU. Jt Comm J Qual Patient Saf. 2017;43(2):62-70.
Deb S, Claudio D. Alarm fatigue and its influence on staff performance. IIE Trans Healthc Syst Eng. 2015;5(3):183-96.
Drew BJ, Harris P, Zègre-Hemsey JK, et al. Insights into the problem of alarm fatigue with physiologic monitor devices: A comprehensive observational study of consecutive intensive care unit patients. PLoS One. 2014;9(10):e110274.
Funk M, Clark JT, Bauld TJ, Ott JC, Coss P. Attitudes and practices related to clinical alarms. Am J Crit Care. 2014;23(3):e9-18.
Joint Commission, The. Hospital: 2018 National Patient Safety Goals. 2018.
Kane-Gill SL, O’Connor MF, Rothschild JM, et al. Technologic distractions (part 1): Summary of approaches to manage alert quantity with intent to reduce alert fatigue and suggestions for alert fatigue metrics. Crit Care Med. 2017;45(9):1481-8.
Karns CM, Isbell E, Giuliano RJ, Neville HJ. Auditory attention in childhood and adolescence: An event-related potential study of spatial selective attention to one of two simultaneous stories. Devl Cogn
Neurosci. 2015;13:53-67.
Konkani A, Oakley B, Penprase B. Reducing hospital ICU noise: A behavior-based approach. J Healthc Eng. 2014;5(2):229-46.
Korniewicz DM, Clark T, David Y. A national online survey on the effectiveness of clinical alarms. Am J Crit Care. 2008;17(1):36-41.
Ruskin KJ, Hueske-Kraus D. Alarm fatigue: Impacts on patient safety. Curr Opin Anaesthesiol. 2015;28(6):685-90.
ant5-Focus on Technology-430


















