The pulmonary artery (PA) catheter aids diagnosis and helps guide therapy by measuring intravascular pressures and cardiac output. For patients with hypotension, heart failure, and respiratory failure, PA catheter use has been the standard of care for more than three decades. Generations of nurses and physicians have spent countless hours learning how to set up, calibrate, and maintain the PA catheter system; take hemodynamic measurements with it; and adjust therapy based on its findings.
But in many—perhaps most—intensive care unit (ICU) situations, the PA catheter is misused, overused, or abused. For one thing, taking accurate measurements with it can prove challenging. For another, these measurements commonly are misinterpreted, leading to incorrect clinical decisions. Many clinicians simply lack proper education, training, or practice to accurately interpret information derived from the PA catheter.
To best serve patients, all ICU team members need to be aware of how and why the PA catheter should be used, its problems and limitations, and its alternatives.
Set-up challenges
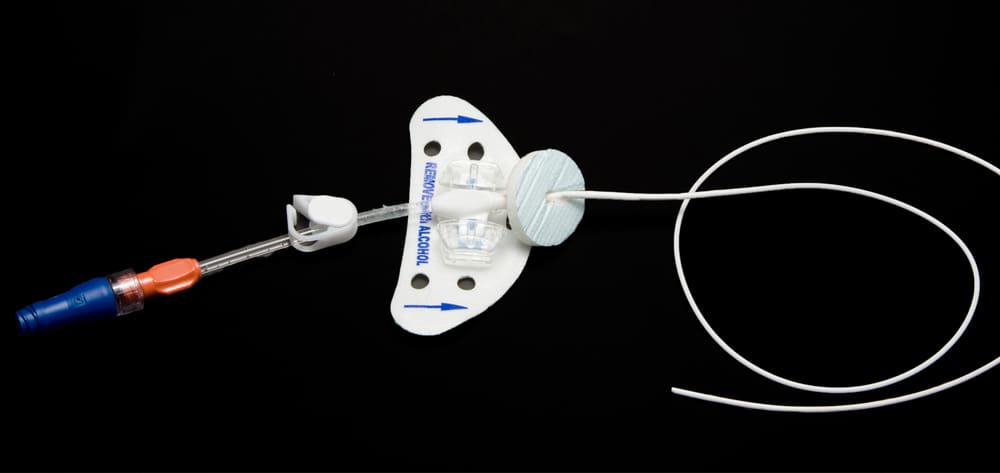
It’s relatively easy to make mistakes when setting up the PA catheter system—and incorrect set-up means inaccurate measurements. The pressure transducer must be properly leveled, with the reference stopcock placed at the phlebostatic axis (at the fourth intercostal space, in the middle of the lateral side of the chest). The catheter must be zeroed with the stopcock open to room air at this level, and monitoring devices must be calibrated accordingly. Unless these steps are done before every set of measurements is taken, true hemodynamic values will be over- or underestimated, leading to flawed interpretation.
Perhaps the most cumbersome approach to maintaining a properly leveled system is to attach the stopcock to an I.V. pole. Unless the patient’s bed always stays at a fixed position and is never raised or lowered, attaching the stopcock to an I.V. pole entails use of a leveling device to align the transducer with the patient’s midchest area. Every time measurements are taken, the equipment must be releveled and rezeroed.
A more reliable and convenient approach is to tape the stopcock and transducer to the patient at the correct level. However, the equipment still needs to be zeroed at intervals. Regardless of the set-up method used, every ICU should have a standardized protocol for system set-up to ensure that hemodynamic measurements are reliable and to help prevent complications.
Potential for overdamping or underdamping
Another source of errors involves pressure waveform transmission from the patient through the tubing and then to the electronic sensor. Caregivers must test damping (which reflects how quickly the oscillating system comes to rest) by flushing the system to high pressure generated by the pressure bag on the flush solution in the circuit.
- An overdamped waveform usually stems from air, blood, clots, or kinks in the tubing and leads to underestimation of systolic and diastolic pressures. (The mean pressure reading is less likely to be affected.)
- Underdamping typically results from long tubing or too many stopcocks in the circuit and leads to systolic pressure overestimation and diastolic pressure underestimation.
Interpretation errors
Even if system set-up and measurements are flawless, a large body of research shows many clinicians don’t know how to interpret measurements correctly. In one study, 496 physicians in 13 U.S. and Canadian healthcare facilities took a 31-question, multiple-choice exam to test their ability to recognize and interpret PA catheter tracings. The results were disappointing: The mean score was only 67% correct answers. Test performance didn’t correlate with the level of the clinician’s training or frequency of PA catheter use or whether the hospitalwas a primary medical school affiliate.
In some cases, simplistic reasoning leads clinicians to misinterpret waveform meanings. The most common misconception is that PA occlusion pressure (PAOP, often called wedge pressure) reflects the patient’s volume status. Many clinicians think low PAOP indicates hypovolemia and high PAOP indicates hypervolemia. But the underlying physiology is more complex. PAOP doesn’t reflect volume status, especially in patients with cardiac or pericardial disease. It doesn’t even reflect left ventricular end-diastolic pressure, as in patients with tachycardia or high pulmonary alveolar pressures or in those receiving positive end-expiratory pressure.
Such incorrect assumptions can lead clinicians to make errors in diagnosis, initial therapy, and maintenance therapy. Clinicians may focus on determining the patient’s PAOP when they should be trying to determine the patient’s fluid status. When making decisions about initial therapy, they may ask themselves, “Should we give fluid or diuretics?” based on whether PAOP is above or below a predetermined level. But patients with hypovolemia, hyper-volemia, or euvolemia may all have the same PAOP. So this measurement must be coupled with clinical assessment and viewed in the context of how it changes after an intervention. Using similarly erroneous assumptions, clinicians may decide to keep PAOP at a certain level when determining maintenance therapy.
Do PA catheters improve patient outcomes?
It’s not easy to prove that any diagnostic or monitoring device—even a stethoscope or pulse oximeter—improves patient outcomes. Unless linked with a beneficial intervention, a piece of equipment won’t change outcome. Yet, clinicians take it on faith that information derived from that equipment can be used to make proper decisions.
However, unlike the stethoscope and pulse oximeter, a growing body of evidence suggests that PA catheter use not only doesn’t help but may harm patients. Several earlier studies looked back at patients in various settings and found an overall higher mortality in those who’d had PA catheters compared to those who didn’t. However, critics of these studies properly maintained that perhaps patients with PA catheters were sicker or their caregivers misinterpreted PA catheter data.
New studies investigating whether PA catheter-directed, protocol-driven therapy is superior to other approaches consistently show it has no benefit—and perhaps increases risks. In a large prospective study of elderly, high-risk patients undergoing major surgery, PA catheter-directed therapy brought no benefit over standard therapy in short-or long-term survival or length of stay. In another multicenter trial, 1,000 patients with acute lung injury or acute respiratory distress syndrome were randomized for hemodynamic management guided by a rigorous protocol using either a PA catheter or a central venous catheter. To avoid criticism that lack of benefit stemmed from inadequate knowledge of PA catheter measurement and interpretation, all study personnel had extensive training in measuring vascular pressure. The researchers found that PA catheter-guided therapy didn’t improve organ function or survival at 60 days and was associated with more complications.
Promoting proper PA catheter use
The major rationale for PA catheter use in the ICU is to improve our understanding of a patient’s physiology so we can make intelligent treatment decisions. PA catheters provide valid measurement of intravascular pressures in the lung but are less than reliable for left ventricular end-diastolic volume or preload.
No diagnostic method can be expected to improve outcome unless its results lead to specific interventions. Despite widespread acceptance of the PA catheter as a tool in managing high-risk perioperative and critically ill patients, its benefits remain unproven, even in recent randomized, prospective, controlled investigations.
Some clinicians will always believe that in the right hands, the PA catheter is an indispensable part of patient management, even if a definitive study eventually shows otherwise. But too many ICU caregivers lack proficiency with it.
We believe the PA catheter should be used only in high-risk patients when clinicians are uncertain about the diagnosis or the first treatment steps. Effective alternatives exist and ICU caregivers need to be familiar with these. Also, every ICU team member should receive education and show proficiency in inserting and maintaining the PA catheter system and acquiring and interpreting data from it. An outstanding educational resource is the Web-based program dedicated to critical care available at www.pacep.org.
Most importantly, healthcare practitioners need to be receptive to new evidence and willing to change our practice when the evidence takes us there. It’s not easy to change old habits. But our patients’ well-being demands it.
Selected references
Fowler R, Cook D. The arc of the pulmonary artery catheter. JAMA. 2003;290:2732-2734.
Iberti T, Fischer E, Leibowitz A, et al. A multicenter study of physician knowledge of the pulmonary artery catheter. JAMA. 1990;12:2933-2940.
Michard F, Teboul J-L. Predicting fluid responsiveness in ICU patients. A critical analysis of the evidence. Chest. 2002;121:2000-2008.
National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. Pulmonary-artery versus central venous catheter to guide treatment of acute lung injury. N Engl J Med. 2006;354;2213-2224.
Vender J. Pulmonary artery catheter utilization: the use, misuse, or abuse. J Cardiothorac Vasc Anesth. 2006;20:259-299.
For a complete list of selected references, see June 2007 references.
Mark J. Rosen, MD, FCCP, FCCM, FACP, is Chief of the Divisions of Pulmonary, Critical Care and Sleep Medicine at North Shore University Hospital in Manhasset, N.Y. and Long Island Jewish Medical Center in New Hyde Park, N.Y.; he is also Professor of Medicine at the Albert Einstein College of Medicine in Manhasset and New Hyde Park. William Senicola, CCRN, RN, is Manager of the Medical Intensive Care Unit at North Shore University Hospital in Manhasset.