Use a tool for consistent, objective, and quantifiable patient assignments.
- Patient assignments can lead to dissatisfaction among nursing staff, especially when they’re not consistent, objective, and quantifiable.
- Dissatisfaction can create barriers to the adaptability and teamwork that are critical to good patient care.
- The patient acuity tool addresses the important issue of unbalanced nurse-patient assignments and helps nurses influence decision-making in their organizations.
Patient assignments can lead to dissatisfaction among nursing staff, especially when they’re not consistent, objective, and quantifiable. This dissatisfaction can create barriers to the adaptability and teamwork that are so critical to good patient care.
In 2016, three RNs on a complex 23-bed medical-surgical unit at Durham VA Health Care System identified a recurring complaint by nursing staff that patient assignments were inconsistent and unequal. An average of five RNs and one charge nurse were assigned five patients per nurse per shift. The nursing assignment system included placing patients in one of two categories: “standard patient” or “involved care” patient. The problem was the subjectivity of these terms; they had no supporting evidence. The result was frustrated nurses, which prompted the unit to develop a process improvement project.
Standardizing handoff communication
The Bedside Mobility Assessment Tool 2.0
Hours per patient day: Understanding this key measure of productivity
Purpose and goals
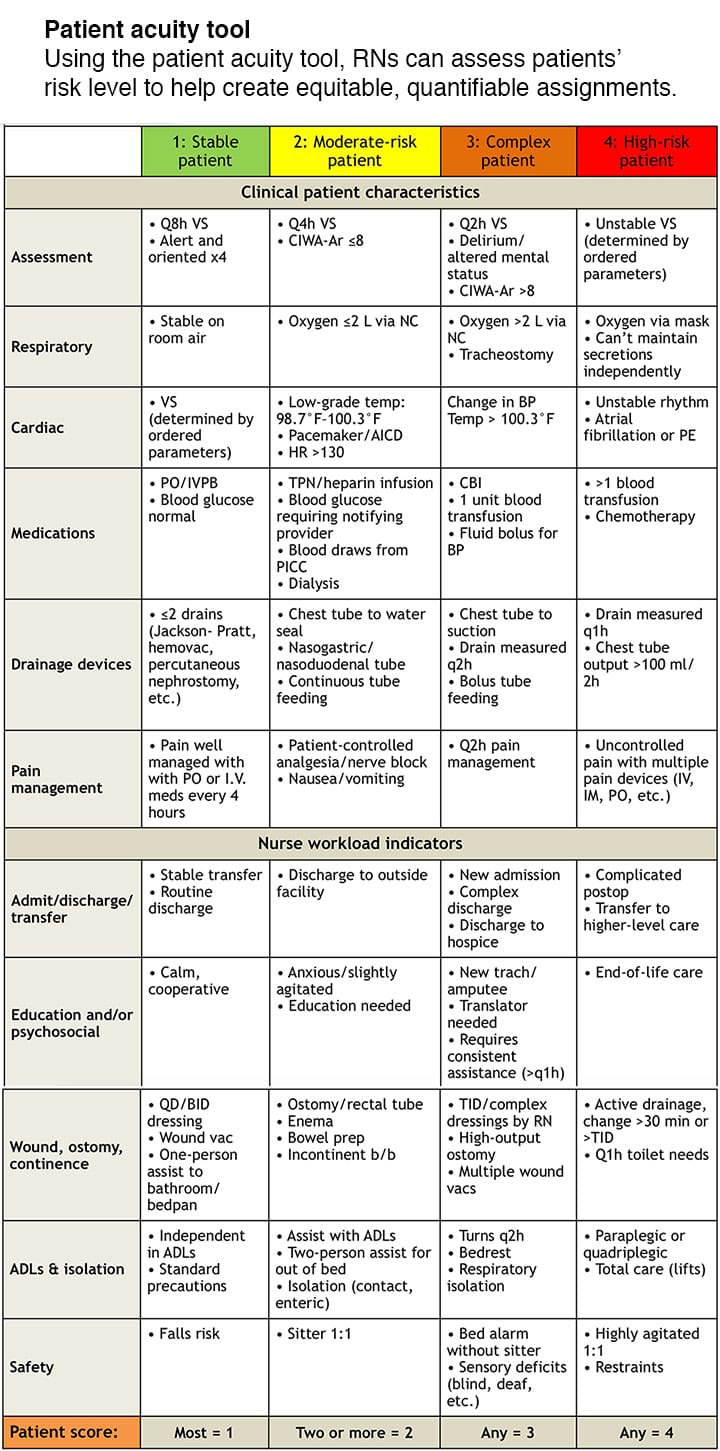
We used evidence-based information to create an objective acuity tool to establish patient assignments. The tool uses both clinical patient characteristics and workload indicators to score patients from 1 to 4 based on acuity level. This approach gives nurses the power to score their patient, then report to the charge nurse so that RN assignments for the oncoming shift are quantifiable and equitable. It also gives them the opportunity to assess the level of patient safety risk.
The goals of the tool are to:
- increase nurse satisfaction with their patient assignment
- increase nurse perception of patient safety by assigning patients with high acuity scores equitably.
The patient acuity tool
Each patient is scored on a 1-to-4 scale (1, stable patient; 2, moderate-risk patient; 3, complex patient; 4, high-risk patient) based on the clinical patient characteristics and the care involved (workload.) Each nurse scores his or her patients, based on acuity, for the upcoming shift and relays this information to the charge nurse, who then assigns patients before the shift change. The handoff report between RNs allows each to validate patients’ current acuity and care needs. (See Patient acuity tool.)
Methodology
Anecdotal reports by the RN staff and our observations prompted the collection of data from staff. Some of the staff comments about the current system included:
- “Why are my patient assignments so unfair?”
- “How will I care for all of my patients effectively?”
- “Involved care is a subjective term.”
We conducted a literature review and eventually combined two existing tools and restructured them to create our acuity tool. Before implementing the process improvement project, we used the newly created tool to assess the current average distribution of total acuity among nurse assignments, and we asked RNs to complete a 10-question survey to measure their satisfaction with patient assignments and perceptions of patient safety. We then taught the RNs how to use the tool and placed color-coded, laminated copies at every nursing computer.
The tool was pilot tested for 28 days. After the first 14 days, we conducted an audit to assess compliance, which revealed that average compliance among all four shifts was 35%. We then collected data on the average distribution of total acuity among nurse assignments. Progress e-mails were sent to staff, and individual follow-ups were held to promote compliance. At the end of the 28 days, we conducted another compliance audit, which revealed an average compliance among all four shifts of 77%, an increase of 220%.
Data
At the end of the pilot study, we reviewed patient assignments before and after implementing the acuity tool to assess their equality, and we surveyed RNs about the two goals we set for the project: improve nurse satisfaction and increase nurse perception of patient safety.
Equality of patient assignments
To determine the equality of nurses’ assignments within a shift, the difference in total acuity between the highest and lowest scoring assignments was obtained. (See RN assignments using acuity tool.)
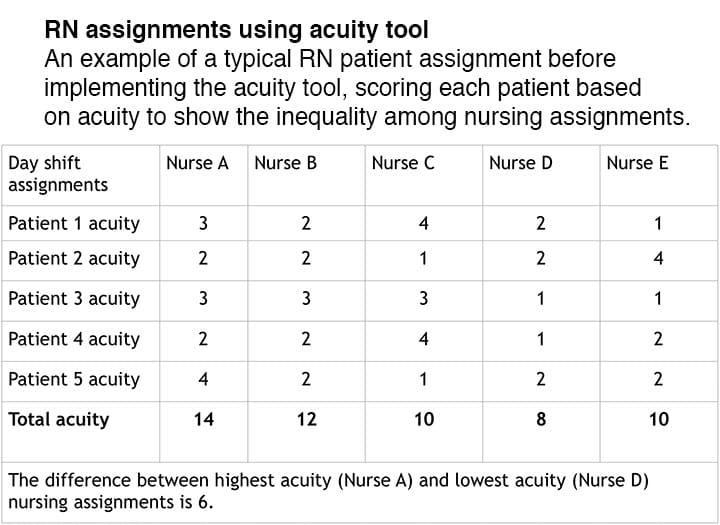
Before implementing the acuity tool, the average distribution of total acuity between highest and lowest nurse assignments for each shift was 4.83 (using a scale of 1 = lowest acuity and 4 = highest acuity). After implementation, the average distribution of total acuity between highest and lowest nurse assignments was 3.06, a 36.6% improvement in equality and accuracy.
Goal 1: Improve nurse satisfaction
Three of the 10 questions in the nurse survey were aimed at nurse satisfaction, including RN perception of patient assignment equality, having input into making assignments, and frequency of feeling overwhelmed with patient assignments. The most significant change occurred with the question “Please rate how frequently you feel overwhelmed with your patient assignment.” Response options were never (1), rarely (2), sometimes (3), frequently (4), and every shift (5). According to the survey, the weighted average of nurse satisfaction was 3.19 before implementing the acuity tool and 2.84 (11% improvement) after.
Goal 2: Increase nurse perception of patient safety
When asked to respond to the statement “I feel like patient safety is a concern when I accept my patient assignment,” RN staff chose from the following options: never (1), rarely (2), sometimes (3), frequently (4), and every shift (5). The weighted average was 3.38 pre-implementation and 3.21 post-implementation, a 5% improvement in RNs’ perception of patient safety. After reviewing the annual performance improvement data, we found no direct correlation between using the acuity tool and patient safety measurements (rate of falls, medication errors, and restraint use). However, by distributing high-acuity patients among nurses, this tool, used in conjunction with other current actions, can reduce the need for patient safety measures such as using sitters and frequent rounding.
Challenges
We attributed many of the challenges faced during the implementation of this project to staff assignment changes during some 24-hour periods. Sometimes patient assignments changed every 4 hours because of differences in nurse shift length, which left the staff with no consistent communication between shifts. The charge nurse would also occasionally take a patient assignment when patient acuity was high and RN census was low, resulting in outliers in data.
Another challenge included RN staff changes during the pilot study, leading to gaps in education about proper use of the tool, decreased feedback, and less data in post-implementation than pre-implementation. As part of our sustainment plan, we’ll incorporate education on the tool in new staff orientation, adapt it to other medical-surgical units in the hospital, and continue quarterly audits to assess compliance.
Benefits
Given the original concern by staff that assignments were unequal, one of the strengths of this acuity tool is that it allows nurses to become stakeholders in making patient assignments. In addition, it also gives the charge nurse an objective way to justify assignment rationale. The tool costs no money to implement and requires no special technology. In addition, it’s noninvasive to the unit’s workflow, easy to implement, and easily adapted to different units and their specific needs. We’ve also found that the tool enhances the shift-to-shift handoff report and that it can be used to assign patients based on nurse competence (novice nurses, expert nurses, etc.).
Striking a balance
The patient acuity tool addresses the important issue of unbalanced nurse-patient assignments and helps nurses influence decision-making in their organizations. Our research found that an objective patient acuity tool on a medical-surgical floor could increase assignment equality, improve nurse satisfaction, and improve nurse perception of patient safety. The tool is now being piloted on other units at this facility, and we’ve received consults from other facilities in the Veterans Affairs Health Care System.
Happiness strategiesUse these strategies to create sustainable happiness.
|
Andrea Ingram is a medical-surgical certified nurse at the VA Health Care System in Durham, North Carolina. Jennifer Powell is a neonatal intensive care unit nurse at Novant Health Hemby Children’s Hospital in Charlotte, North Carolina.
Selected references
Chiulli KA, Thompson J, Reguin-Hartman KL. Development and implementation of a patient acuity tool for a medical-surgical unit. Academy of Medical-Surgical Nurses. 2014;23(2):1, 9-12.
Kidd M, Grove K, Kaiser M, Swoboda B, Taylor A. A new patient-acuity tool promotes equitable nurse-patient assignments. American Nurse Today. 2014;9(3):1-4.



















24 Comments.
Hello, I am working on my DNP project and wondering if I could utilize the PAT here during my study citing it appropriately?
Thank you
Nikki
would like to know more about this classification tool, is it still in use or has it been revised? can it be used without copywrite restrictions? is it electronically available
Yes, you can use it but must source the tool appropriately.
I am interested to know how to utilize this acuity tool. I have several nurses complain about assignments, this might be something that our unit could utilize to better assignments.
My name is Tijuana L Parker and we want to use your tool on our unit to see if we can balance the assignments better and improve nurse satisfaction.
Hi Mrs. Andrea Ingram, and Jennifer Powell,
I would like to ask if there is any educational material on how di you roll out your acuity tool.
Dear Mrs. Andrea Ingram, and Jennifer Powell
My name is Myriam Valdema, a DNP student. Thank you for such a fantastic study. I am writing my final project on a patient-acuity tool’s effect on job satisfaction in a medical-surgical Unit. We are currently using the block method to make assignments, and it is not working well for the nurses. With your permission, I would like to use the tool to provide better patient assignments while improving patients’ safety.
Thank you
Sincerely, Myriam Valdema BSN, RN
Thank you for the great article Andrea Ingram and Jennifer Powell.
I am writing to seek permission to reuse the tool for our tertiary hospital. Let me know the psychometric properties of the tool or Has it been tested for validity and reliability.
Sincerely
Dr.Asha Raj Sudha
Dear Mrs. Andrea Ingram, and Jennifer Powell,
Thank you for a very intersting study. We are interested in implementing it in our hospital.
May we ask :
1) Is it applicable to all types of patient population or restricted to medical surgical as the the title of the article suggests?
2) Has it been tested for validity and reliability and can be safely used to assess the patients acuity.
3) Has it been successfuly in other hospitals?
4) Is there a copyright if want to use?
We started a project on my unit about four years ago using EPIC to created a tool for our surgical trauma progressive care. Working with our EMR nurse team, we were able to customize the tool to fit our patient population. If you would like more information, please let me know.
Patrice, I would love to know how you utilized EPIC to create an acuity tool. I am currently working on finding or creating one for my department. I would love if you could reach out to me. My personal email is wiels1987 at gmail. Thank you.
Interesting article, thank you for acknowledging and taking action to help improve a system. It would be ideal to have a universal acutiy tool that all units can adapt to their speciality. I was wondering how you than use this tool to decide how many staff you require on the ward? If you have so many orange and red level patients, are you able to aquire more staff? Or are you only using this tool to allocate patients equitably between the 5 staff you have?
I was wondering if we would be able to reference the acuity tool in an EVB project we are doing?
This is an interesting article, but I think the use of quantitative measures such as means on ordinal scales is incorrect. First, the score (1, stable patient; 2, moderate-risk patient; 3, complex patient; 4, high-risk patient) is made to be ordinal, therefore, the interpretation “the average distribution of total acuity between highest and lowest nurse assignments for each shift was 4.83” is not appropriate and should not be used. The difference between “stable patient”, “moderate-risk patient” and “complex patient” are not equal. In other words, one cannot assume that the difference between responses is equidistant even though the numbers assigned to those responses are. The same interpretive problem is present for the question “Please rate how frequently you feel overwhelmed with your patient assignment”. The response options were never (1), rarely (2), sometimes (3), frequently (4), and every shift (5). The comment : “the weighted average of nurse satisfaction was 3.19 before implementing the acuity tool and 2.84 (11% improvement) after.”, is also incorrect. I would suggest reporting the percentage of each classes and the median (1). This would be transparent and avoid false interpretations if the answers were clustered at the high and low extremes.
Secondly, I understand the need to have an objective tool and I also chase this goal, but when I read the table “RN assignments using acuity tool”, I come to the conclusion that it is not at all objective and that the nurse’s classification is completely subjective. Either the tool needs to be less interpretation-free and have more quantitative criterias or the nurses need to have the same interpretation of each criteria before using the tool.
I want to thank you for your work as it is a great start and hope you continue to enhance this potentially powerful tool.
Thank you
Vincent Morissette-Thomas, Statistician and Data Scientist
1. Sullivan, Gail M., and Anthony R. Artino Jr. “Analyzing and interpreting data from Likert-type scales.” Journal of graduate medical education 5.4 (2013): 541-542.
Nice article on acuity. Many years I developed numerous acuity systems from P.I.C.U., to ED and Psychiatric units.
I am interested in using a Patient Acuity tool for my DNP project. Can I use this tool?
Thank you.
Catherine Bell MSN RNC
Dear Mrs. Andrea Ingram, and Jennifer Powell,
I am interested in using a Patient Acuity tool for my project. Can I use this tool?
Thank you.
Joy
Thank you Great article. I was wanting to contact author about the possibility of using this tool.
I am writting in regards to “patient acuity tool on a medical surgical unit”
I am currently connected with a regional hospital (government owned) here in the philippines with a bed capacity of 800 but in reality it is way more than that since we are not allowed to refuse a patient since we are the end refferal hospital in our region.. my hospital have not adapted any tool on patient assignment that most often led to nurse job unsatisfaction and burnt out. And i think your study will be of great help. But before my hospital can adapt this, it has to be grounded with a study and so I will be making a study on this and would like to use also your survey with some revisions that is applicable to us if you could allow me. Thank you in advance.
Thank you all for the responses to the article! I am sorry it has taken me this long to respond, but I would love to provide the survey used. Unfortunately, I’m only able to find 6 of the 10 questions (my account used for the online survey was deleted) but I hope these questions help you.
Re: Liz Doll, I’m so glad you would find this tool helpful. You are more than welcome to adapt our tool to fit your patient population. I hope it works out well for your staff!
1. How long have you been a nurse?
2. How long have you been a nurse on 6A? (the name of our unit)
3. In my opinion, I feel that patient assignments are equal between nursing staff. (Strongly agree, agree, neutral, disagree, strongly disagree.)
4. In my opinion, I feel like I have input into making the nursing assignments. (Strongly agree, agree, neutral, disagree, strongly disagree.)
5. Please rate how frequently you feel overwhelmed with your patient assignment. (Frequently, sometimes, rarely, never.)
6. I feel like patient safety is a concern when I accept my patient assignment. (Every shift, frequently, sometimes, rarely, never.)
Loved this study and was wondering if there’d be a way to get a copy of the survey used? Thank you!
Is there a way to get a copy of the survey questions used? This is a great article!
Becky
Thank you for this insightful article. Our hospital is expanding beds and we have been using this tool to ensure our new units are properly staffed. With your permission, our team would like to make slight modifications to this tool to better fit our unique patient population. Please let me know your thoughts!
I am writing in regards to “Patient acuity tool on a medical-surgical unit” (Morrow and Powell, 2018). I believe patient acuity is a critical aspect to take into consideration when looking at staffing and nursing assignments. I agree with method the article used, creating a tool to score patient acuity. It is important to have an objective way to determine the acuity and fairly assign patients to a nurse. Having a balanced assignment benefits not only nurses by decreasing their workload, but also extends to the patients by giving them better outcomes.
As a bedside nurse I have experienced overwhelming, unbalanced patient assignments. Being stretched thin forces me to be more task-oriented rather than patient centered, as I would prefer. Several months ago the unit I work for started utilizing a tool similar to the one mentioned in the article. By giving us an objective way to rate the acuity of a patient it lead to more balanced the assignments. It gave us more of a say in the assignments, the charge nurses ask us our opinions on our patient group and if they need to be separated for the next shift. This makes us feel as though we have a voice and give the charge nurse an objective way to fairly make assignments (Morrow, 2018).
Overall, RNs who rated their assignments as appropriate were more likely to be satisfied with their jobs, intend to stay on their current units, and deliver quality care to patients than those who rated their assignments as inappropriate.
Registered nurses who said that their assignments were appropriate are more likely have higher job satisfaction and deliver higher quality care to patients as opposed to nurses who said their patient assignments were inappropriate and unbalanced (Choi, 2018). I find that in my own practice, a balanced mix of acuity within an assignment group I am able to spend more face-to-face time with each patient as opposed to having a group of patients who are all considered high acuity. Utilizing a patient classification system is a low cost tool that nurse leaders can ensure that nurses are receiving equal assignments.
Sincerely,
Carrie Young, RN
References
Choi, J (2018). Registered Nurse Perception of Patient Assignment Linking to Working Conditions and Outcomes. Journal of Nursing Scholarship, 50(5). Retrieved from https://doi-org.liblink.uncw. edu/10.1111/jnu.12418
Morrow, A. & Powell, J. (2018). Patient acuity tool on a medical-surgical unit. American Nurse Today, 13(4). Retrieved from https://www.myamericannurse.com/patient-acuity-meidcal-surgical-unit