In July, the American Nurses Association (ANA) hosted its first in-person Sharps Injury (SI) Prevention Stakeholder meeting. Experts, advocates, specialists, and frontline nurses from varied backgrounds with global renown convened to discuss the state of sharps injuries and needlesticks in U.S. health care. With hepatitis C infections and associated comorbidities, including metabolic syndrome, diabetes, and coinfection with hepatitis B, HIV or multidrug resistant organisms, at an all-time high, especially among baby boomers, renewing focus and making concerted efforts to reduce sharps injuries and bloodborne and infectious disease exposures is time critical.
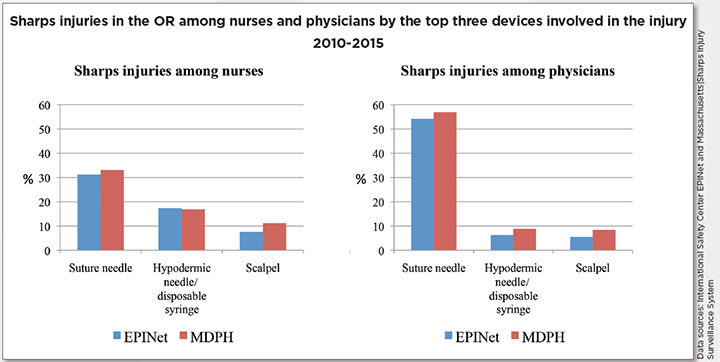
 An analysis of publicly reported sharps injury surveillance data from the Massachusetts Department of Public Health (Massachusetts Sharps Injury Surveillance System [MSISS]) and the International Safety Center (Exposure Prevention Information Network [EPINet]) illustrates that employees working in the operating room (OR) sustain more injuries from contaminated needles and sharp instruments—and therefore occupational exposures to bloodborne pathogens—than any other single location in the healthcare setting. In fact, an average of almost 40% of all injuries occur in the OR compared to all other departments in facilities contributing data to both MSISS and EPINet.
An analysis of publicly reported sharps injury surveillance data from the Massachusetts Department of Public Health (Massachusetts Sharps Injury Surveillance System [MSISS]) and the International Safety Center (Exposure Prevention Information Network [EPINet]) illustrates that employees working in the operating room (OR) sustain more injuries from contaminated needles and sharp instruments—and therefore occupational exposures to bloodborne pathogens—than any other single location in the healthcare setting. In fact, an average of almost 40% of all injuries occur in the OR compared to all other departments in facilities contributing data to both MSISS and EPINet.
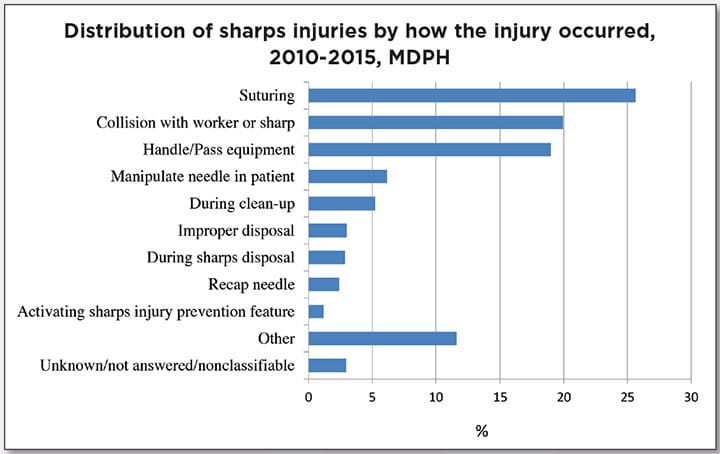
Nurses sustain about 15% of injuries in the OR even though they are not likely to be the original user of the device (the instrument was not being held or used by them). This means that injuries are occurring with hand-to-hand passing of devices, inside of the operative field during the use of an instrument by the surgeon, from devices left on surfaces or floors, and from devices that are not safely contained in a sharps disposal container. Protecting the health and wellness of surgical teams is an essential element to not just the safety of staff, but also the safety of the patient and the fiscal viability of the healthcare organization.
When employees indicate they were injured in the OR, about 80% record that it was a device without a sharps injury prevention feature. Even though the OSHA Bloodborne Pathogens Standard requires the use of engineering controls for needles and sharp medical devices in all departments of health care where there is anticipated occupational exposure to blood or other potentially infectious materials, uptake has been slowest in the OR and in other surgical settings.
Reducing preventable sharps injuries will require continuous concerted efforts and should include the following, especially for high-risk areas like the OR and surgical settings:
- improving the review, evaluation, and uptake of devices with engineered sharps injury prevention features
- more and ongoing feedback on devices and safer practices from frontline users
- accurate and improved quality of recordkeeping
- incident reporting free from retaliation
- ongoing focus on workers’ rights and employer responsibility
- building and maintaining strong cultures and climates of safety
- increased availability and accessibility of safer devices and personal protective equipment
- high-quality and frequent training and education
- worker empowerment and autonomy to report unsafe conditions
- feedback loops to manufacturers and distributors for in-servicing and future device design needs.
 ANA SI Prevention Stakeholders agree that focusing on reducing incidents in the OR needs to be a high priority and a continuing focus for the upcoming year. Workgroups will explore many avenues for improving SI prevention, including the creation of a “Safe OR Pilot” program, media and press outreach, creation of accreditation and licensing standards, and formalizing terminology for consistency of messaging and impact.
ANA SI Prevention Stakeholders agree that focusing on reducing incidents in the OR needs to be a high priority and a continuing focus for the upcoming year. Workgroups will explore many avenues for improving SI prevention, including the creation of a “Safe OR Pilot” program, media and press outreach, creation of accreditation and licensing standards, and formalizing terminology for consistency of messaging and impact.
Successful strategies will require collaborations between frontline nurses, managers, administrators, academicians, engineers, and advocates from professional associations, member organizations, manufacturing, distributors, researchers, and advocacy groups. The ANA SI Prevention Stakeholder group looks forward to continuing to play a role in fostering this collaboration in an effort to protect the health and safety of healthcare workers.
Editor’s note: The authors wrote this as a summary of proceedings from the ANA Sharps Injury Prevention Stakeholder Meeting, held at ANA in July 2017.
Karen A. Daley is a nationally recognized sharps safety expert and policy advocate and served as president of the American Nurses Association from 2010-2014. Angela K. Laramie is an epidemiologist and has been the coordinator of the Sharps Injury Surveillance Project at the Massachusetts Department of Public Health since 2001. Amber Hogan Mitchell is the president and executive director of the International Safety Center. The Center is a 501c3 nonprofit organization that provides the Exposure Prevention Information Network (EPINet®) to healthcare facilities around the world for free.
December 2017 Frontline FINAL