Find out if you have what it takes to pursue this fast-paced career path.
Takeaways:
- Radiology nursing is a little-known specialty that’s not always an obvious career option for nurses.
- They influence care in a variety of settings, including academic medical centers, community hospitals, outpatient imaging centers, and freestanding radiology clinics.
- Nurses have an important role to play before radiology procedures, during, and after.
TECHNOLOGY and imaging advances have made radiology a rapidly growing field. Percutaneous minimally invasive approaches aided by radiologic techniques are improving outcomes and reducing patient pain, recovery times, and hospital stays. Image-guided biopsies have largely  replaced expensive surgical procedures such as exploratory laparotomies, and procedures like radiofrequency ablations provide a treatment option for liver cancer patients who aren’t candidates for surgery.
replaced expensive surgical procedures such as exploratory laparotomies, and procedures like radiofrequency ablations provide a treatment option for liver cancer patients who aren’t candidates for surgery.
As radiology grows, so does the demand for radiology nurses who possess the knowledge, skills, and behaviors that drive and contribute to optimal patient outcomes. Nurses outside of radiology have little exposure to this field, and nursing students rarely have an opportunity to complete a radiology clinical rotation. This has kept radiology nursing a little-known specialty and not an obvious career option.
Why become a radiology nurse?
Radiology nurses influence care in a variety of settings, including academic medical centers, community hospitals, outpatient imaging centers, and freestanding radiology clinics. Radiology is a dynamic environment that allows nurses to work in different modalities and sub-specialties such as ultrasound, magnetic resonance imaging (MRI), computed tomography (CT), interventional radiology, neuro-interventional radiology, and radiology-oncology. Many nurses enjoy their autonomy and variety of care responsibilities while working as an integral part of a small team of skilled providers.
Radiology nurses have a broad skill set and care for patients across the lifespan at various acuity levels. In one encounter, they may administer a glucagon injection for an MRI patient, in the next respond to an emergency contrast media reaction, and later take part in a high-risk interventional procedure by transfusing blood in a patient with significant bleeding. Nurses who thrive in this environment are flexible and comfortable with a changing routine.
How do radiology nurses impact patient care?
Radiology nurses are systems thinkers who manage environmental and system resources for effective care. They use the nursing process and integrate the knowledge and skills from other nursing specialties to ensure optimal and safe care. They have the rapid assessment, patient flow, and coordination skills of ambulatory and emergency department (ED) nurses; they’re experts at patient positioning, comfort, and fall prevention similar to operating room nurses; and they manage complex care (for example, hemodynamic monitoring and vasoactive drip titration) in the same way intensive care unit (ICU) nurses do.
Radiology nurses are experts at administering minimal to moderate sedation and/or analgesia for patient comfort and pain management. The care they provide is evidence-based and governed by federal and state laws and regulations. Their practice also is guided by professional organizations such as the Association for Radiologic and Imaging Nursing (ARIN) and the American College of Radiology.
Patient-centered care
Radiology nurses are a vital component of the radiology triad (radiologist, radiology technologist, and radiology nurse). They keep patients in the center of the triad and provide a compassionate, supportive, and therapeutic environment. They facilitate patient education, explaining to patients what they should expect before and after the radiology procedure. Radiology nurses are vigilant and responsive to patient and family needs, and they provide impartial culturally competent care.
Safety
Radiology can be a high-risk specialty with patient acuities ranging from stable to critically ill. Patients can rapidly deteriorate, and harm can result from falls, pressure injury, overexposure to radiation, and infections. Radiology nurses vigilantly assess patients for any physiologic changes and address their complex needs. Although patients are in radiology nurses’ care for a short time, these nurses advocate for patient safety and appropriate care.
Nursing care in radiology generally begins before the patient is physically in the department. Depending on the setting, patients may be outpatients only or a mix of inpatients and outpatients. The radiology nurse establishes rapport with outpatients by phone a day or two before the procedure. That call involves screening (including checking for allergies and reviewing current medications) and education (including NPO requirements and what to expect on the day of the procedure). Throughout each patient encounter, the radiology nurse communicates with radiologists and other members of the care team to ensure patient needs are met.
Before the procedure. The radiology nurse completes preprocedure checklists and reviews assessment information. He or she ensures safe medication practices and understands medication class routes, dosages, and effects, consulting with a pharmacist as needed.
During the procedure. The radiology nurse closely monitors the patient, ensures comfort, and administers ordered medications and other therapies as needed.
After the procedure. Patients are sent to a paranesthesia care unit (PACU), an inpatient unit, or an intra-departmental recovery area. After the patient is discharged, the radiology nurse calls him or her to rule out postprocedure complications and reinforce teaching. For inpatients, the periprocedure process is similar to the outpatient process, but the radiology nurse primarily communicates with the patient’s bedside nurse for prescreenings and other care needs. Before transfer to radiology, the radiology nurse verifies with the bedside nurse that preprocedure checklists are completed and orders are executed.
Radiology nurses also respond to emergencies and adverse events and are expected to participate in the root cause analysis of those events for quality and safety monitoring and performance improvement.
Efficiency
Radiology nurses coordinate care. They serve as liaisons between the radiology department and other care areas such as inpatient units, pharmacy, PACU, anesthesia, and infection prevention. They promote collaboration and encourage team member contribution toward optimal patient care. They also facilitate throughput to reduce wait times and prevent avoidable delays.
Operational flow challenges faced by radiology nurses include add-on cases, late or no-show patients, and walk-in patients. Magnifying these challenges are the non-direct care activities—including problem-solving, phone calls, setup, cleanup, and transport—that radiology nurses perform. This time isn’t always factored into productivity because of the episodic nature of patient encounters. Nurses have to continually triage and prioritize care, taking into account urgent and emergent cases or changes in patient condition that require a higher level of care or inpatient admission.
What education and training are required?
Entry-level education for radiology nurses is an associate degree in nursing and an RN license. Because of patient complexity and range of acuity, nurses usually are required to have basic life support and advanced cardiac life support certifications (pediatric advanced life support is required for those who care for children).
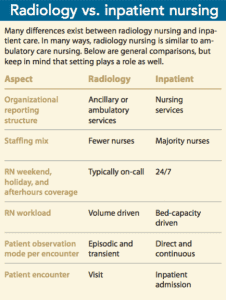
Most nurses who work in radiology transfer from the ICU, ED, or PACU. Initially, the environment presents a steep learning curve, even for seasoned nurses who are experts in their previous specialty. The different modalities, number of procedures, departmental skill mix, level of autonomy, and lack of routine contribute to that learning curve. (See Radiology vs. inpatient nursing.) However, once nurses acclimate, they rarely want to leave the specialty.
Historically, radiology administrators have hired only experienced nurses, but as nurse residency and new graduate programs emerge, more new graduates are entering radiology. ARIN recommends a 6-week orientation for experienced nurses and up to 12 weeks for new graduates. ARIN has an orientation manual for radiology nurses and a core curriculum that can be used as resources for ideal training and education.
Nurses can obtain Certified Radiology Nurse (CRN®) specialty certification, which demonstrates dedication to the specialty and the nursing profession as a whole. Radiology nurses also can benefit from joining ARIN, which provides access to the Journal of Radiology Nursing and continuing education opportunities. Other professional organizations that are of value to radiology nurses are the Association of periOperative Registered Nurses, American Association of Critical-Care Nurses, the American Academy of Ambulatory Care Nursing, and the Society of Interventional Radiology. (See Radiology nursing roles.)
Consider pursuing a unique specialty
The radiology environment is fast-paced, and the specialty of radiology nursing is rapidly growing. Radiology nurses are integral to providing exceptional care for every patient. This unique specialty offers autonomy and opportunities to care for a variety of patients using a range of emerging technologies.
Muriel Moyo is a radiology nurse manager at Keck Medical Center of the University of Southern California in Los Angeles.
Selected references
American Nurses Association, Association for Radiologic and Imaging Nursing. Radiologic & Imaging Nursing: Scope & Standards of Practice. Silver Spring, MD: American Nurses Association; 2013.
Association for Radiologic and Imaging Nursing. Orientation Manual for Radiologic and Imaging Nursing. 2nd ed. Herndon, VA: Association for Radiologic and Imaging Nursing; 2014.
Cefaratti M, Benninger R, Nguyen R. Implementing a hospital-based radiology nursing orientation program for new graduate pediatric nurses. J Radiol Nurs. 2013;32(4):170-9.
Chittle MD, Vanderboom T, Borsody-Lotti J, et al. An overview of clinical associate roles in the neurointerventional specialty. J Neurointerv Surg. 2016;8(3):323-7.
Gross KA. Core Curriculum for Radiologic and Imaging Nursing. 3rd edition. Herndon, VA: Association for Radiologic and Imaging Nursing; 2014.
Grossman VA. Hot topics: Get them in, keep them safe, get them out, and make everyone happy while you do it! J Radiol Nurs. 2011;30(3):137-8.
Jeffery AD, Werthman J. Successful orientation strategies for radiology nurses. J Radiol Nurs. 2015;34(2):94-9.
Penzias A, Cadman S, Sullivan A, McIntosh K. Mentoring the nurse of the future: Clinical nurse specialist students in the radiology setting. J Radiol Nurs 2015;34(3):150-6.
Penzias, A. Management and leadership: The next generation: Introducing prelicensure students to radiology nursing. J Radiol Nurs. 2015;34(2):115-6.
Sousa MF. Management and leadership: An agile approach to new nurse orientation: How one hospital created a sustainable orientation plan for newly hired radiology nurses. J Radiol Nurs. 2013;32(1):45-7.



















6 Comments.
Thank you for this. The field is related to a couple of other “invisible” specialties like nuclear medicine and radiation oncology where there are shared histories and technologies. Nurses are also seeing an increasing role in these areas but schools do not offer information on these topics during core training.
i am a radiology nurse who work in HK, thank you for your sharing.
it provides me lots of “stimulations” in how to improve our current setting and future development !
I really like the information which is shared in this blog about the interventional radiologist Radiology nurses influence care in a variety of settings, including academic medical centers, community hospitals, outpatient imaging centers, and freestanding radiology clinics. Radiology is a dynamic environment that allows nurses to work in different modalities and sub-specialties such as ultrasound, magnetic resonance imaging (MRI), computed tomography (CT), interventional radiology, neuro-interventional radiology, and radiology-oncology. Many nurses enjoy their autonomy and variety of care responsibilities while working as an integral part of a small team of skilled providers. The radiology environment is fast-paced, and the specialty of radiology nursing is rapidly growing. Radiology nurses are integral to providing exceptional care for every patient. This unique specialty offers autonomy and opportunities to care for a variety of patients using a range of emerging technologies.
Excellent article capturing almost all the essence of being a Radiologic & Imaging Nurse! Congratulations!!!!
The post is very informative. It is a fact that Radiology is not only useful across a variety of settings but also offers vast opportunities to work in different modalities and sub-specialties. I believe, there is a lot in this Post for nurses who aim to advance their career in Radiology field. Thank you for sharing.
Well Done !
Alberto F. Pernudi
City of Hope National Medical Center
Director of Radiology