Catheter-associated urinary tract infections (CAUTIs) are the most frequent type of healthcare-acquired infection, accounting for up to 80% of hospital-acquired infections. CAUTIs can lengthen hospital stays, increase morbidity and mortality, and raise healthcare costs. The Centers for Medicare & Medicaid Services no longer reimburses hospitals for additional costs generated by CAUTIs. This article reports on a pilot study of an evidence-based intervention to reduce CAUTIs.
Guidelines for care
National and international guidelines on CAUTI prevention have existed for years. Various prevention strategies beyond the standard guidelines have been studied, with mixed results. Meanwhile, CAUTI incidence continues to climb. Recent recommendations from the Centers for Disease Control and Prevention’s Healthcare Infection Control Practices Advisory Committee (HICPAC) appropriate catheter use and maintenance.
The need for better documentation
Multiple studies have found prolonged catheterization greatly increases the CAUTI risk, with each catheter day raising the infection risk 3% to 10%. Yet catheter duration rarely is monitored daily. Most nursing documentation flow sheets feature a small area for genitourinary assessment, but accurate documentation of catheter assessment, duration of use and condition, and tubing securement methods commonly is missing.
Physician reminders
One study found a simple intervention to remind physicians to remove unnecessary catheters can decrease CAUTI rates. Another revealed that prewritten stop orders involving six criteria are acceptable for continued catheter use; if none of the criteria are met, nurses are required to remove the catheter.
What nurses can do to reduce CAUTIs
To meet the Joint Commission’s new patient safety goal on CAUTIs, which went into effect January 1, healthcare providers must follow evidence-based interventions. The evidence suggests a primary factor in CAUTI development is catheterization duration. In light of this, a colleague and I developed a UTI prevention (UTIP) bundled protocol of several preventive measures. The bundle protocol was adapted from a bladder bundle protocol developed by members of the Keystone Center for Patient Safety & Quality associated with the Michigan Health & Hospital Association.
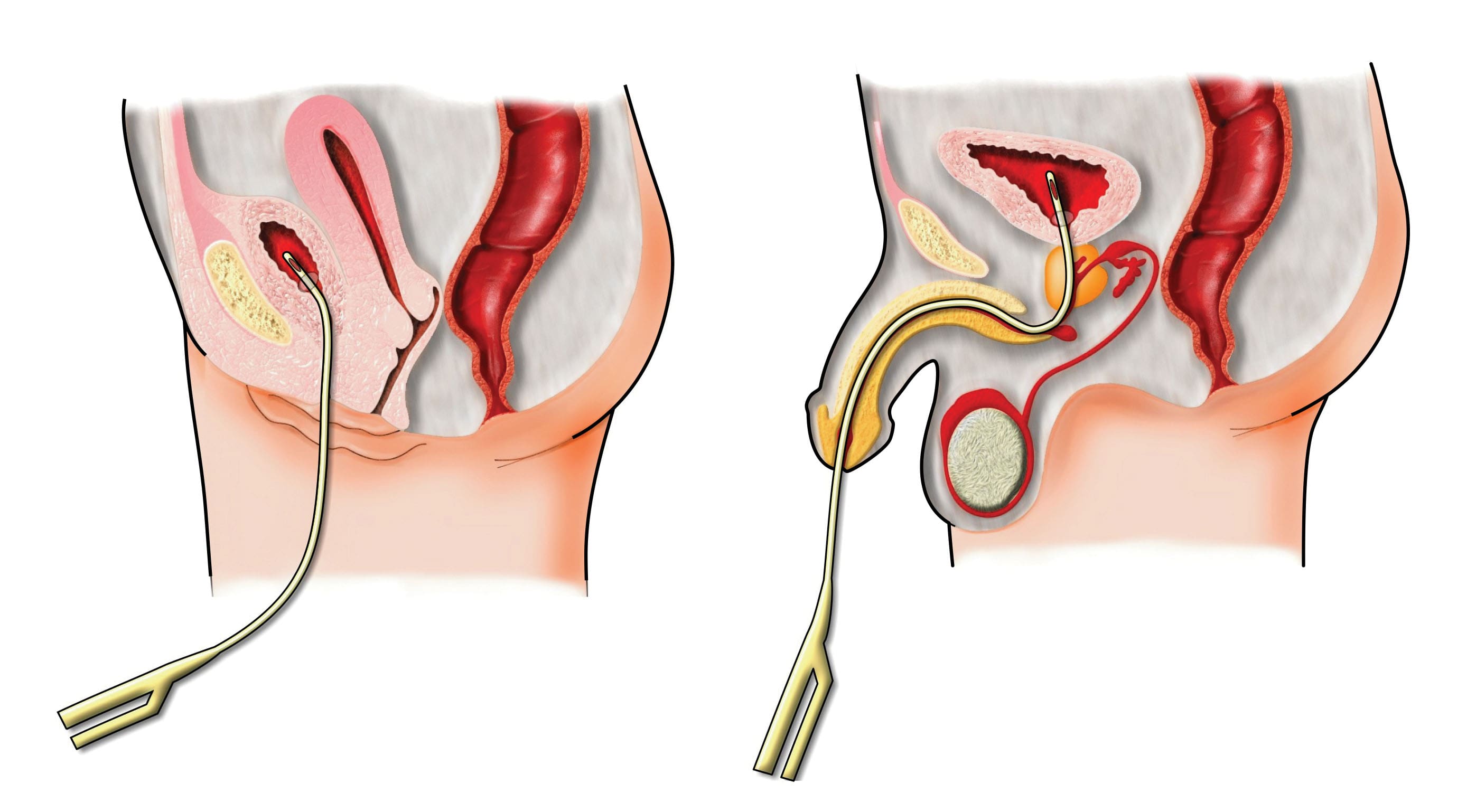
The UTIP bundle consists of four nursing elements related to catheter use. Our pilot study evaluated the efficacy of combining these elements into a comprehensive bundled protocol and set of guidelines. The elements are:
- use of the smallest possible antimicrobial-impregnated catheter (#14 or #16 Fr)
- daily monitoring of the number of patients on the nursing unit who have catheters, as well as the type, size, and duration of each catheter
- use of a specified area in nurses’ bedside charts or the electronic medical record for documenting daily assessment of catheter condition and securement method and potential for catheter removal
- development and use of a daily reminder system to alert physicians of the need to evaluate the patient’s urinary status and consider catheter removal. The charge nurse can stamp a reminder message in the physician’s progress-notes section of the chart; the reminder also can be discussed during daily rounds.
We also developed a list of appropriate reasons for continuing catheterization based on HICPAC guidelines. (See Appropriate reasons for continuing catheterization b y clicking the PDF icon above.) After providing education for nurses and physicians, we conducted this pilot study for 3 months. Results showed the UTIP protocol reduced catheter days by nearly 1.5 patient days (from 5.3 to 3.8 days). Nurses’ compliance with all protocol elements was nearly 100%.
Recommendations
As a nurse, you’re largely in control of your patients’ catheterization duration. Even if your employer lacks a protocol for monitoring catheter use and reducing duration, you can follow the UTIP bundle protocol by:
- always using the smallest catheter possible and documenting its insertion date and time
- taking extreme care when securing the catheter, and never elevating the tubing or drainage bag above the insertion site
- monitoring and documenting catheterization duration and assessing the need for continuation daily
- reminding the physician of the catheter and discussing possible removal if no appropriate reason for continuing catheter use exists.
Visit www.AmericanNurseToday.com for a complete list of references.
Brian T. Conner is an assistant professor at the Medical University of South Carolina College of Nursing in Charleston.