Acute-care settings present challenges for PI prevention, but solutions exist
By Jan Powers, PhD, RN, CCNS, CCRN, NE-BC, FCCM, and Corinne (Cori) Ames BSN, RN, CMSRN
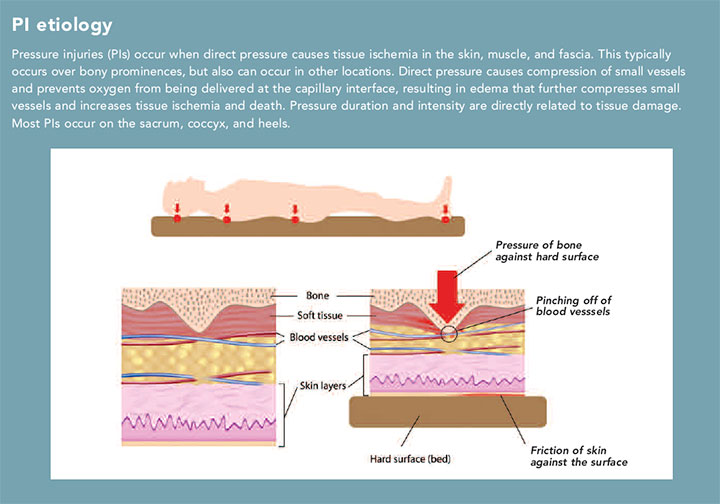
Nurses are on the frontlines of pressure injury (PI) prevention, assessment, and management. Understanding PI risks and causes and having a firm grasp on the tools and skills required for accurate assessment help to ensure successful patient outcomes. (See PI etiology.)
In this article, we’ll discuss nursing considerations related to PIs within the acute-care setting, including methods to enhance patient care.
Risk factors
While the most significant PI risk factor is reduced movement or immobility, several factors can place patients at risk, including decreased perfusion and oxygenation, increased skin moisture and temperature, friction and shear, decreased sensory perception, hemodynamic instability, vasoactive medications, intensive care unit (ICU) length of stay, surgery, and overall health status. Pressure from medical devices—such as catheters, and I.V. and endotracheal tubes—also can cause PIs. And patients with existing PIs are at increased risk for others.
Nutritional deficiency and advanced age have been shown to increase the risk of PIs. Aging decreases dermal thickness and sensory perception, which can lead to more rapid tissue injury but leave patients less likely to respond to tissue cues to change position. Poor nutritional status may result in decreased protein, rendering tissue more susceptible to the effects of pressure.
Intensive nursing care decreases complications and improves patient outcomes. Studies have suggested that PI development also can be affected by the number of nurses and time spent at the bedside. A structured approach that includes comprehensive risk assessment is recommended to identify PI risk. Use a reliable and valid tool appropriate to the specific patient population, and implement interventions specific to the patient’s needs based on the scoring criteria used.
 Acute-care challenges and solutions
Acute-care challenges and solutions
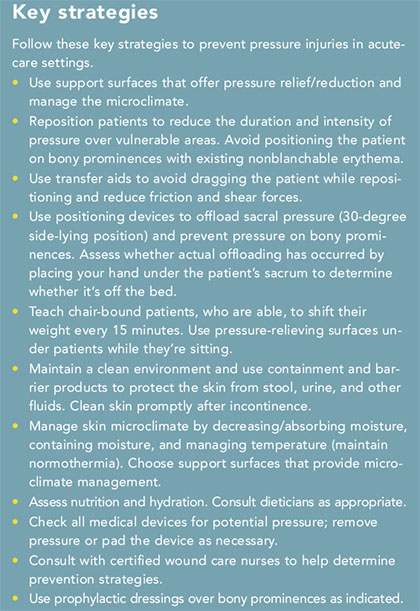
Nurses in acute-care settings often juggle multiple needs for multiple patients, some with several comorbidities, which requires impeccable organizational skills. All acute-care settings should have a comprehensive prevention program that includes risk assessment, skin care, pressure redistribution, friction and shear management, incontinence/moisture management, nutritional assessment and interventions, education (for both clinical staff and patients), and communication. (See Key strategies.) However, specific settings—ICU, emergency department (ED), and operating room (OR)—have their own unique challenges and solutions. Here’s an overview; you can learn more by reading related articles in this special report.
Emergency department
Patients in the ED often present with life-threatening or serious health conditions that take priority over skin assessment. However, while patients are in the ED, they’re typically cared for on transport carts that may not have the same types of pressure-reduction mattresses as hospital beds. Some facilities have protocols to add additional pressure-reducing surfaces for high-risk
patients in the ED. Also, because many patients move out of the ED quickly, no protocol exists for turning patients at least every 2 hours. Take note of patients who stay longer than 2 hours and reposition them as needed.
Operating room
Unique challenges in the OR include operating tables and required patient positioning. OR tables are rigid and can cause significant PIs if they’re not appropriately padded or if the patient isn’t properly positioned. Similarly, medical devices used during surgery should be padded and carefully positioned to prevent PIs. Because patients can’t be repositioned during surgery, assess for potential pressure areas and patient risk, and request prevention accommodations before surgery begins.
Intensive care unit
Patients in the ICU must contend with multiple medical devices that may cause PIs, as well as conditions and medications that may cause vasoconstriction and reduce blood flow to the skin. The resulting decrease in perfusion and oxygenation may make patients more susceptible to PIs. Patients in the ICU generally require multiple medications for hemodynamic instability, which may make repositioning a challenge due to blood pressure changes. You can still shift patients to relieve pressure, just use smaller adjustments and turns. In addition, patients in the ICU are at increased risk of malnutrition and require interdisciplinary coordination to implement early nutritional support. They also may experience temperature variations—either hypothermia, which decreases perfusion, or hyperthermia, which increases moisture. Maintain normothermia when possible.
Nursing considerations
The most important aspect of nursing care is diligent assessment and implementation of prevention strategies. Assessments should be performed at admission, by each nurse on each shift, when patients are transferred, and at discharge. Many organizations have adopted two-person skin assessment at admission. The skin assessment score should then direct you to the appropriate prevention strategies.
 Use protocols, guidelines, order sets, or care plans that outline appropriate nursing care measures based on risk assessment and prevention strategies. The bundle approach is a comprehensive, collaborative solution for PI prevention or reduction. In two recent studies, PIs were decreased significantly after implementing a bundle of prevention strategies.
Use protocols, guidelines, order sets, or care plans that outline appropriate nursing care measures based on risk assessment and prevention strategies. The bundle approach is a comprehensive, collaborative solution for PI prevention or reduction. In two recent studies, PIs were decreased significantly after implementing a bundle of prevention strategies.
Prophylactic dressings, such as a polyurethane foam dressing on bony prominences, may help prevent PIs in anatomical areas frequently subjected to friction and shear. These dressings also can be used to protect skin from medical devices. Choose prophylactic dressings designed to allow for regular skin assessments. For example, they should have soft silicone borders that are easy to lift for routine skin checks without creating tape burns or other injuries.
Other research-based measures include standardized communication tools to enhance interdepartmental collaboration, and support surfaces—such as mattress overlays and specialized bed surfaces—that alter the microclimate by regulating the rate of moisture evaporation and heat dissipation.
A centerpiece of care
PIs can occur in any acute-care environment. You and your colleagues should understand the factors that place patients at increased risk for PI and be knowledgeable about prevention strategies. A one-size-fits-all prevention option doesn’t exist, so the best approach is comprehensive, collaborative bundling of multiple interventions individualized to each patient. Make PI awareness and education a centerpiece of your nursing care.
The authors work at Parkview Health in Fort Wayne, Indiana. Jan Powers is the director of nursing research and professional practice. Corinne (Cori) Ames is nursing services manager 3—surgical and inpatient wound care.
Selected references
Anderson M, Finch Guthrie P, Kraft W, Reicks P, Skay C, Beal AL. Universal pressure ulcer prevention bundle with WOC nurse support. J Wound Ostomy Continence Nurs. 2015;42(3):217-25.
Brindle CT, Wegelin JA. Prophylactic dressing application to reduce pressure ulcer formation in cardiac surgery patients. J Wound Ostomy Continence Nurs. 2012;39(2):133-42.
Bryant RA, Nix DP. Acute and Chronic Wounds: Current Management Concepts. 5th ed. St Louis, MO: Mosby, Inc; 2016.
Cooper KL. Evidence-based prevention of pressure ulcers in the intensive care unit. Crit Care Nurs. 2013;33(6):57-66.
Joint Commission Resources, The Source, Joint Commission Compliance Strategies. Under Pressure: Preventing perioperative pressure injuries 15(11):1-22.
Molon JN, Estrella EP. Pressure ulcer incidence and risk factors among hospitalized orthopedic patients: Results of a prospective cohort study. Ostomy Wound Manage. 2011;57(10):64-9.
National Pressure Ulcer Advisory Panel. Prevention and treatment of pressure ulcers: Clinical practice guideline. 2014.
National Pressure Ulcer Advisory Panel. Pressure injury prevention points. 2016.
Swafford K, Culpepper R, Dunn C. Use of a comprehensive program to reduce the incidence of hospital-acquired pressure ulcers in an intensive care unit. Am J Crit Care. 2016;25(2):152-5.
Yusuf S, Okuwa M, Shigeta Y, et al. Microclimate and development of pressure ulcers and superficial skin changes. Int Wound J. 2015;12(1):40-6.
ANT0518_Dabir_TakeAction