Weak evidence for AHA/ACC guidelines
Between 1984 and 2008, the American Heart Association/American College of Cardiology (AHA/ACC) issued 53 guidelines with 7,196 recommendations. But according to a recent study, about half of the recommendations are based on expert opinion, case studies, or standard of care—not on data from multiple clinical trials or meta-analyses. The study’s findings are based on the grading system currently used by the AHA/ACC guidelines, which classifies the strength of evidence and recommendations.
Parenteral drug errors in the ICU
A recent study of about 1,300 adults in 113 intensive care units (ICUs) in 27 countries, including the United States, analyzes self-reported errors in parenteral drug administration. Here are some of the findings:
- For every 100 patient-days, 75 errors occurred.
- The most common error was administering drugs at the wrong time.
- Most errors occurred during routine situations—not crises.
- The likelihood of errors was higher when patient-nurse ratios were higher.
- The likelihood of errors was lower when infusion equipment was routinely checked at shift changes and when a critical incident reporting system was used.
Changes to screening recommendations
The U.S. Preventive Services Task Force has updated the recommendations on screening patients for type 2 diabetes and colorectal cancer. For type 2 diabetes, the old recommendation was to screen patients who had hypertension and hyperlipidemia. The new recommendation is to screen patients with blood pressure readings of 135/80 mm Hg or higher without regard to lipid levels.
For colorectal cancer, the recommendation established in 2002 was to screen all people older than age 50. The new recommendation is that people ages 50 to 74 should be screened in one of three ways: every year with high-sensitivity fecal occult blood testing, every 10 years with colonoscopy, or every 5 years with flexible sigmoidoscopy and interval high-sensitivity fecal occult blood testing.
Nurse-led quality improvement
The Robert Wood Johnson Foundation has selected 16 hospitals for its Aligning Forces for Quality program called “Transforming Care at the Bedside Collaborative.” According to experts, this collaborative isn’t a traditional quality improvement program because of its primary focus on engaging nurses and other frontline staff to develop and lead the quality improvement efforts.
Ideas for transforming care come not from the hospital’s executive suite or quality improvement staff, but from those who spend the most time providing direct care to patients. Nurse-led teams identify where change is needed on their unit, suggest and test potential solutions, and decide whether and how those innovations should be implemented.
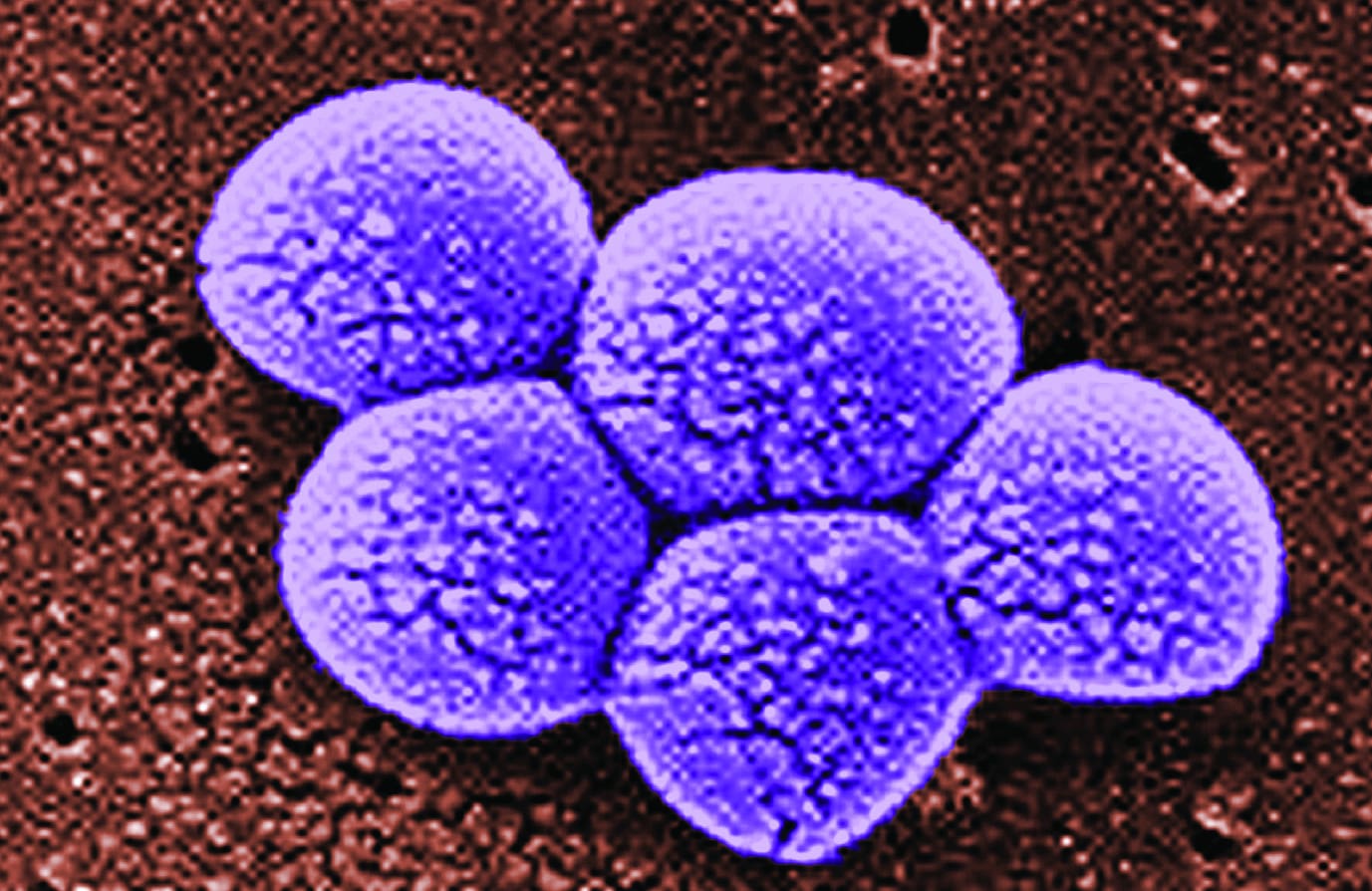
A drop in central line–associated MRSA infections
Since 2001, central line–associated infections caused by methicillin-resistant Staphylococcus aureus (MRSA) have declined steadily in adult ICUs, according to an analysis of the Centers for Disease Control and Prevention’s data.
Data from nearly 1,700 ICUs show that the overall incidence of central line–associated MRSA infections fell by about 50% between 1997 and 2007, with most of the decrease beginning in 2001. The incidence of all central line–associated bloodstream infections also fell during the study period.
Upcoming symposium on relationship-based care
The inaugural symposium on relationship-based care will take place July 28 to 31, 2009, at the Turning Stone Resort in Verona, New York. Relationship-based care places personal relationships between caregivers and patients and their families at the center of care delivery. The model for this approach provides tools for organizing care and effecting change as well as guidance for transforming the cultures of healthcare institutions from depersonalized, schedule-driven systems into person-centered sources of individualized care.
Review of Clostridium difficile infection
A review of C. difficile infection published in the Journal of the American Medical Association includes pathogenesis, risk factors, clinical presentation, prevention, and treatment. Among the highlights:
- Risk factors for the infection include antimicrobial use, hospital admission, old age, and impaired immunity.
- Using antimicrobials prudently can reduce the risk of infection.
- Discontinuing antimicrobial therapy that’s causing a mild infection may resolve it.
- The treatment of choice for moderate-to-severe infections is oral metronidazole (Flagyl).
- The first-line treatment for severe infections is oral vancomycin (Vancocin).