ONE IN FIVE patients diagnosed with acute pancreatitis will develop recurrent acute pancreatitis, and one in three of them will develop chronic pancreatitis (CP), which increases the risk for pancreatic cancer.
Chronic pancreatitis also may be associated with other complications, such as pseudocyst formation, bile duct or duodenal obstruction, pancreatic ascites or pleural effusion, splenic vein thrombosis, and pseudoaneurysms. (See At a glance: Acute pancreatitis.)
Total pancreatectomy (TP)—a surgery whose frequency has significantly increased over the last 20 years—is a final resort for patients who can’t achieve pain and symptom relief with other treatment modalities including less extensive surgery.
The surgery is irreversible and leaves the patient with no pancreatic endocrine and exocrine function. Because insulin-secreting islet of Langerhans cells (islet cells) are removed along with the pancreas, insulin production ceases. Though still considered an experimental surgery, TP with islet cell autologous transplantation (TP-IAT) is an option that preserves insulin-making capabilities. Successful islet cell transplantation may give patients better glycemic control, fewer complications from diabetes, and improved quality of life after surgery—effects that reduce the morbidity and mortality associated with a total pancreatectomy.
Chronic pancreatitis
A study by Kesseli and colleagues shows that CP causes more than 56,000 hospital admissions in the United States annually. According to Schrope, chronic pancreatitis is “progressive and unrelenting” and can take a severe toll on patients’ quality of life.
CP results from progressive fibrotic destruction of the pancreas, which can occur as a result of various factors, including intraductal chronic obstruction (for example, from tumors or stones) and autoimmune disorders (such as Sjögren syndrome and primary biliary cirrhosis). Although alcohol is the most common cause of CP, about 30% of cases are idiopathic.
Patients typically report abdominal pain that often radiates to the back, with the pain ranging from mild to severe and debilitating. Patients may also experience nausea, vomiting, diarrhea, and weight loss.
Unlike acute pancreatitis, which is diagnosed based on elevated pancreatic enzyme levels (amylase and lipase), CP is diagnosed by reviewing the patient’s clinical history and risk factors (which include recurring acute pancreatitis, lifestyle choices such as alcohol consumption and smoking, congenital small pancreatic duct, hyperlipidemia, and gallstones), and via imaging. Pancreatic enzyme levels may be tested, but with CP they may not be elevated. Complete blood count electrolytes, and liver function tests also may be normal. In cases of intra-pancreatic compression, fibrosis, or cancer, serum bilirubin, and alkaline phosphatase may be elevated.
Contrast-enhanced computed tomography may show calcification, ductal dilatation, enlarged pancreas, and fluid collection near the pancreas. Magnetic resonance cholangiopancreatography is becoming a test of choice because it better shows calcification and pancreatic duct obstruction consistent with CP. Endoscopic retrograde cholangiopancreatography (ERCP) is widely used and enables providers to use therapeutic intervention, such as stenting.
CP interventions and management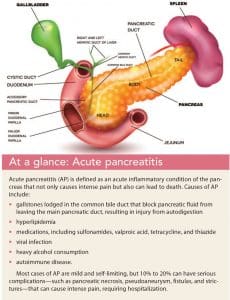
CP usually is treated with a “step-up” approach, beginning with medication therapy and life-style changes.
Debilitating abdominal pain is present in 90% of patients with CP, making pain management a priority. Pain management usually consists of oral analgesia, starting with nonsteroidal anti-inflammatory drugs (NSAIDs) and progressing to opioids. Unfortunately, some patients become opioid tolerant and dependent because of the severe pain they experience. Antidepressant and anticonvulsant medications also can be used to relieve neuropathic pain. If oral analgesics aren’t successful, celiac nerve blocks may be considered.
If medication fails to control symptoms, endoscopic intervention is an option with ERCP. Endoscopic decompression and stent placement can be performed for patients with CP caused by obstructions or narrowing of the pancreatic duct. If both medical and endoscopic interventions fail to manage symptoms, surgery can be considered. TP is used for patients with chronic pancreatitis to relieve unremitting pain.
Islet cell transplantation
One of the most lifestyle-altering side effects of a total pancreatectomy is the development of type 3c diabetes caused by the loss of islet cells. However, with TP-IAT, islet cells can be retrieved from the pancreas and reinjected into the patient intraoperatively to maintain some insulin production.
After the pancreas is removed, it’s sent to the lab for retrieval of islet cells. The surgeon then injects the cells into the portal vein (insulin from the pancreas normally is secreted into the portal circulation), where they circulate into the liver. The portal vein is easy to access for injection and has the capacity for a large-volume infusion of islet cells.
Although the islet cells begin releasing insulin soon after transplantation, patients will require supplemental insulin until the cells are fully functional. The cells’ viability is tested through serum C-peptide levels. Half of the patients who receive TP-IAT will have viable islet cells 6 months after surgery. About one-third of those patients become independent from insulin, one-third will have partial islet cell function requiring small amounts of insulin, and the remainder will have graft failure and become insulin dependent.
Nursing considerations
Nursing care after TP-IAT includes pain management, nutrition, and glucose control.
Pain management
One of the biggest challenges of TP-IAT is postoperative pain management. Patients should be counseled preoperatively about the difference between acute, postoperative pain and the chronic pain they have been living with. Explain that surgery will create additional short-term pain, but it will ultimately reduce chronic pain.
Before surgery, most patients have been living with chronic, intractable pain for years, and some have developed opioid tolerance. Even with adjuvant therapies, such as anticonvulsants, NSAIDs, antihistamines, antianxiolytics, and antidepressants, managing postoperative pain can be difficult.
Patients who suffer from chronic pain typically are well versed in medication administration. They may demand specific timetables and be particular about how drugs are administered. Some patients develop opioid tolerance due to CP pain, and others may display substance misuse behaviors that must be appropriately managed. Over time, TP may eliminate the chronic pain associated with the condition, but managing postoperative pain will remain a challenge until patients are fully weaned from opioids.
Advocate for and promote a team approach to pain management. Weaning patients off opioids will require time and support from the primary surgery and pain-management teams, nursing, nutrition, social work, and in some cases psychiatry. Consistent surgical team communication about the plan of care and keeping the patient involved are critical to successful outcomes and decreased length of stay.
Overall, studies show that pain is improved after TP-IAT, narcotic use decreases, and quality of life improves. Wilson and colleagues showed that narcotic independence was achieved in 55% of their patients 1 year after TP-IAT and 73% after 5 years. In addition, 92% of patients reported overall health improvement 1 year after surgery. Weaning patients off all narcotics is a slow process, and it won’t be accomplished during hospitalization. As primary caregivers at this crucial time, nurses must encourage safe use of opioids and work with patients toward the goal of eventually achieving opioid independence. Sutherland and colleagues emphasize that “the inability to wean off narcotics is not a treatment failure when quality of life improved after TP-IAT.”
 Nutrition
Nutrition
Many patients with CP experience anxiety and severe nausea, which result in loss of appetite, impaired digestion, and malnutrition. Patients who’ve been living with CP are already at risk for malnutrition because of malabsorption and associated nausea and vomiting. They may already have received percutaneous endoscopic gastrostomy tubes for supplemental tube feeding or central lines for total parenteral nutrition before surgery.
After TP-IAT, GI motility dysfunction may occur, causing nausea and vomiting; patients may require supplemental feedings. Patients should be referred to an inpatient nutritionist or dietitian to help with education about proper nutrition. If feasible, an endocrinology provider also should follow these patients to further assist with education on diabetes management and insulin administration.
The goal for patients after TP-IAT is to return to a solely enteral diet. Like pain management, this process will be gradual and include antiemetic medications to enhance oral intake. Patients also will require lifelong pancreatic enzyme replacement with each meal to maintain optimal nutritional status and prevent steatorrhea.
Glucose control
Islet cells are sensitive and can easily die, so closely monitor patients’ glucose levels after surgery. (See Glucose monitoring preserves islet cells.) Patients also will need to learn how to monitor their own glucose after discharge. Start this education before surgery and continue it throughout the hospital stay. Patients should be proficient at checking glucose levels, counting carbohydrates, and injecting insulin before they’re discharged. Also teach patients and families how to identify signs and symptoms of hypo- and hyperglycemia.
Monitoring, management, education
TP-IAT success requires careful monitoring, management, and patient education provided by an interdisciplinary team. The primary goal of surgery is chronic pain relief, but with islet cell transplantation, complete insulin dependence can be prevented. TP-IAT doesn’t guarantee insulin production and symptom relief, and even successful transplantations may offer only a few years of insulin production. This surgery is high risk, complex, and irreversible, but for many patients, it can offer a better quality of life.
The authors work at New York–Presbyterian/Columbia University Irving Medical Center on a surgical oncology and med/surg floor specializing in hepatobiliary and colorectal surgery. Kimberly Rivera is a patient care director, Amanda Rosenburg is a clinical nurse II, and Kristen Burns is a clinical nurse III, bone marrow transplant.
Selected references
Bhayani NH, Enomoto LM, Miller JL, et al. Morbidity of total pancreatectomy with islet cell au-to-transplantation compared to total pancreatectomy alone. HPB. 2014;16(6):522-7.
Huffman, JL, Obideen K, Wehbi M. Chronic pancreatitis. Medscape. July 15, 2019. emedicine.medscape.com/article/181554-overview
Kesseli SJ, Smith KA, Gardner TB. Total pancreatectomy and islet autologous transplantation: The cure for chronic pancreatitis? Clin Transl Gastroenterol. 2015;6:e73.
Kreimer N. Pancreatic diseases and islet cell transplantation: Implications for life care planning. J Nurse Life Care Plan. 2016;16(2):40-7.
Lew D, Afghani E, Pandol S. Chronic pancreatitis: Current status and challenges for prevention and treatment. Dig Dis Sci. 2017; 62(7):1702-12.
McCance KL, Huether SE. (2019). Pathophysiology: The Biologic Basis for Disease in Adults and Children. 8th ed. 2019; St. Louis, MO: Elsevier.
Muratore S, Freeman M, Beilman G. Total pancreatectomy and islet auto transplantation for chronic pancreatitis. Pancreapedia: Exocrine Pancreas Knowledge Base. February 20, 2015. pancreapedia.org/reviews/total-pancreatectomy-and-islet-auto-transplantation-for-chronic-pancreatitis
National Institute of Diabetes and Digestive and Kidney Diseases. Pancreatic islet transplantation. niddk.nih.gov/health-information/diabetes/overview/insulin-medicines-treatments/pancreatic-islet-transplantation
National Institute of Diabetes and Digestive and Kidney Diseases. Pancreatitis. niddk.nih.gov/health-information/health-topics/liver-disease/pancreatitis/Pages/facts.aspx
Radomski M, Zureikat AH. Total pancreatectomy and islet cell autotransplantation: Outcomes, controversies and new techniques. JOP. 2015;16(1):1-10.
Schrope BA. Total pancreatectomy with autologous islet cell transplantation for chronic pancreatitis: Current challenges. Presented at Pancreas Symposium 2018: Current Controversies in Benign Pancreatic Disease; March 22, 2018.; New York City, NY.
Schrope B. Total pancreatectomy with autologous islet cell transplantation. Gastrointest Endosc Clin N Am. 2018;28(4):605-18.
Sutherland DE, Radosevich DM, Bellin MD, et al. Total pancreatectomy and islet autotransplantation for chronic pancreatitis. J Am Coll Surg. 2012;214(4):409-24.
Wilson GC, Sutton JM, Abbott DE, et al. Long-term outcomes after total pancreatectomy and islet cell autotransplantation: Is it a durable operation? Ann Surg. 2014;260(4):659-65.