Proper primary and secondary securement can reduce complications, increase patient comfort, and save money.
Takeaways:
- Millions of peripheral IVs and central venous catheters are inserted every year.
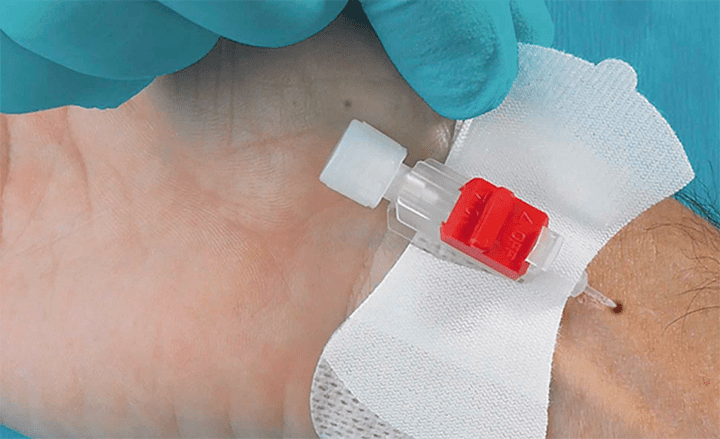
- Securement choices include several types of tape, transparent dressings, sutures, engineered securement devices (ESDs), subcutaneous ESDs, and medical cyanoacrylate tissue adhesives.
- Decisions related to securement should be considered equally as important as the choice of the catheter itself.
Editor’s note: A vital part of a clinician’s responsibility for vascular access is effective stabilization and securement of the device or tubing to reduce the risk of complications. We invited an interprofessional panel of clinicians to share their expertise in stabilization and securement so that readers of American Nurse Today have the knowledge they need to ensure the safety of patients who have a vascular access device (VAD). Carol Czajka, BSN, RN, CPN, VA-BC, and Anne Marie Frey, BSN, RN, VA-BC, CRNI, work at Children’s Hospital of Philadelphia, where they are clinical experts for the vascular access service. Gregory Schears, MD, is a professor of anesthesiology and vascular access expert at the Mayo Clinic in Rochester, Minnesota.
 Why is it so important to stabilize and secure VADs and associated tubing?
Why is it so important to stabilize and secure VADs and associated tubing?
Schears: Proper stabilization and securement is critical to the maintenance and function of all VADs. When a catheter is secured, the forces to retain it are greater than the forces to remove it. This dynamic situation can change quickly with the application of increased force on the I.V. tubing or catheter, which can result in dislodgement.
Czajka: Catheter stabilization prevents the inadvertent movement of the VAD. It lowers the risk of mechanical phlebitis and possible infiltration from the lack of pistoning movement, catheter-related infections from pathogens on the skin migrating into the tract during catheter movement, and loss of the catheter.
Catheter stabilization in pediatric patients is particularly challenging. Take, for example, the 16-year-old patient with developmental delays who had a peripherally inserted central catheter (PICC) in her right upper extremity for antibiotic therapy. When the patient got up during the night to use the bathroom, she stepped on her I.V. tubing, causing her PICC to migrate 9 cm, which required repositioning. The patient had an adhesive primary securement device in place, but not any secondary securement devices. If secondary securement had been used, the force applied to the PICC line would have been absorbed by the secondary securement and not the catheter’s primary securement, which may have prevented the migration.
As vascular access nurses, Anne Marie and I assess VADs at the bedside daily. It’s not uncommon for us to see situations similar to the case of the 16-year-old patient. We find peripheral venous catheters (PVCs) bent at 90-degree angles, kinked, or pulled out, and central venous catheters (CVCs) partially or totally dislodged, with cuffs exposed at the insertion site. This generally happens due to the weight of I.V. tubing and other attachments; catheters or I.V. tubing getting caught on clothing, bed rails, and under the wheels of strollers or wheelchairs; and simple patient tugging.
The most common preventive theme missing from all of these situations is the lack of adequate primary securement and no secondary securement.
Frey: Millions of PVCs and CVCs are inserted annually, and securement of these devices has become an issue of utmost importance. Multiple catheter securement choices are available, including several types of tape, transparent dressings, sutures, engineered securement devices (ESDs), subcutaneous ESDs, and medical cyanoacrylate tissue adhesives.
How do you define stabilization and securement?
Schears: The Infusion Nurses Society (INS) Standards of Practice refers to anchoring a VAD as stabilization and to anchoring of I.V. tubing as securement. Either way, it’s a means to anchor a catheter or tubing to the skin to reduce or prevent movement and maintain its intended functionality.
Catheter securement also can be divided into primary and secondary. Primary catheter securement (or what the INS refers to as stabilization) directly holds the catheter in place on the skin. Secondary securement acts as an additional anchor for the infusion set tubing or extension set to reduce any force the primary securement receives when energy is applied to the tubing by accident or rapid patient movement.
The secondary securement is as important as the primary: No primary stabilization can withstand the forces applied when I.V. tubing becomes trapped in the bed rail during a patient transfer. Without the secondary securement “shock absorber,” the primary stabilization can fail, resulting in a lost catheter.
The quality of VAD stabilization directly impacts the functionality, duration of dwell, and likelihood of a complication for a given catheter. The strength of adhesive-based securement systems depends on the quality of the skin surface and skin prep, the aggressiveness of the adhesive, and the surface area of contact of the device. Devices that keep the catheter or tubing off the skin and on top of the securement device tend to perform better than those that sandwich the catheter between the dressing and the skin due to better skin surface area contact.
What lines need to be secured?
Frey: Based on the definition and rationale for securement, all lines, whether PVCs or CVCs, should be secured. This is especially crucial when placing an infusion line in anatomic areas of greater movement, such as the antecubital veins and saphenous veins in the foot, and for patients who are at greater risk of unintentional dislodgment, including those who are confused, combative, or developmentally challenged, or have experienced changes in mental status, as well as neonates, infants, and toddlers. It can’t be emphasized enough that proper securement prevents complications of I.V. catheters, whether peripheral or central, and promotes patient comfort and safe patient outcomes.
Schears: I completely agree—all lines need both primary and secondary securement. Without this approach, you significantly increase the risk of accidental dislodgement and other complications. Decisions related to securement should be considered equally as important as the choice of the catheter itself.
What should nurses consider when evaluating securement options?
Czajka: According to the 2016 Infusion Therapy Standards of Practice, use of ESDs to stabilize and secure VADs promotes consistent practice among clinicians to reduce VAD motion that can lead to complications, reduce interruption of necessary infusion therapy, and decrease cost of care. Nurses should consider the following points when choosing and evaluating the proper ESD for their patients.
- The ESD should be available in a wide variety of sizes for all populations. They should not be mechanically altered in any manner not recommended by the manufacturer. Doing so could cause potential patient harm.
- Decisions about the most appropriate method for VAD selection and securement include patient age, skin turgor and integrity, previous adhesive skin reactions or injuries, and any type of drainage at the insertion site.
- The ESD should not impede vascular circulation or delivery of the prescribed therapy, damage the catheter, or be a source of needlestick injuries. And it should be gentle to the skin.
- The ESD should not interfere with assessing and monitoring the access site. When assessing and monitoring the access site, check the ESD for intactness and potential complications. Monitoring should be completed per national standards and hospital policies, which usually are based on age, device, and individual patient needs.
Once the ESD is in place, nurses should:
- assess the integrity of the ESD with each dressing change and change the ESD according to the manufacturer’s recommendations and/or hospital policies. Remove all old adhesive before replacing the ESD to allow for appropriate skin antisepsis. Be aware of the risk of medical adhesive–related injuries associated with the use of or removal of adhesive- based ESDs. Devices that are designed to stay in for the life of the VAD should be removed and replaced when stabilization is no longer achieved.
- never re-advance a dislodged or displaced VAD into a vein. Peripherally placed VADs that become dislodged should be removed. Assess dislodged central VADs for tip position, infusion therapies, and other influencing factors. Then stabilize the VAD at the current position; in some cases, a new catheter insertion may be warranted.
What is the evidence supporting the use of ESDs?
Schears: Several clinical studies show the advantages of ESDs compared to the old standards of tape and suture. One large prospective product trial [Schears] compared tape to ESDs for short PIVs and found a 67% reduction in catheter complications, 76% reduction in restarts, and a cost savings of $277,000 in the ESD category compared to tape control.
Another prospective, randomized study by Yamamoto and colleagues compared an ESD to suture and found equivalent quality of securement with a trend toward fewer overall complications, a reduction in bloodstream infections, and no needlestick injuries compared to the suture group.
Several other studies have compared various securement devices. Interestingly, bench studies assessing pull strength of various ESDs seem to predict clinical performance rather well and can be used as a surrogate until clinical data become available.
What are your final thoughts about stabilization and securement?
Czajka: Vascular access securement is of utmost importance in the care and management of patients’ catheters in both the inpatient and outpatient environments. It’s a crucial part of maintaining any VAD and should be assessed and discussed at daily rounds.
Approximately 95% of all patients admitted to the hospital require some form of VAD for treatment and therapies. By providing proper primary and secondary securement, we can decrease complications such as infiltration, phlebitis, infections, catheter migrations, and unintentional dislodgments. We can preserve vessels by preventing frequent PIV restarts or the need to rewire and replace CVCs, an outcome that is important to the care of all patients, particularly those with long-term or lifelong dependency on VAD therapies. And we can improve outcomes in patient comfort and satisfaction.
Frey: Remember every day to be astute, assess your patients’ VADs, and use your ESDs. Our goal is to provide safe, complication-free, comfortable care to our patients. Save the veins.
Selected references
Alexander M, Corrigan A, Gorski L, Hankins J, Perucca R, eds. Infusion Nursing: An Evidence-Based Approach. 3rd ed. St. Louis, MO: Saunders; 2010.
Kornbau C, Lee KC, Hughes GD, Firstenberg MS. Central line complications. Int J Crit Illn Inj Sci. 2015;5(3):170-8.
Infusion Nurses Society. Infusion therapy standards of practice. J Infus Nurs. 2016;39(suppl 1):S1-S159.
Schears GJ. Summary of product trials for 10,164 patients: Comparing an intravenous stabilizing device to tape. J Infus Nurse. 2006;29(4):225-31.
Yamamoto AJ, Solomon JA, Soulen MC, et al. Sutureless securement device reduces complications of peripherally inserted central venous catheters. J Vasc Interv Radiol. 2002;13(1):77-81.
This article is supported by an unrestricted educational grant from Tidi Products (tidiproducts.com). Dr. Schears is a consultant for Tidi.