Quick action prevents respiratory failure.
Takeaways:
- Acute cardiogenic pulmonary edema occurs with reduced cardiac muscle efficiency.
- Decreased pump function results in increased pulmonary venous and capillary hydrostatic pressure, which allows fluid to accumulate in the lung interstitium and interfere with gas exchange.
- Impaired gas exchange can lead to acute type 1 respiratory failure.
RONALD BARRETT* is admitted to the medical telemetry unit after arriving in the ED after 2 days of nocturnal dyspnea and mild chest pressure. Mr. Barrett, who’s 68 years old, can’t speak in complete sentences because of conversational dyspnea, and he’s using accessory muscles to breathe. He has a history of hypertension, hypercholesterolemia, and angina. His home medications include diltiazem, baby aspirin, furosemide, atorvastatin, and nitroglycerin (NTG) sublingual (S.L.) as needed, and his admitting diagnosis is heart failure.
he’s using accessory muscles to breathe. He has a history of hypertension, hypercholesterolemia, and angina. His home medications include diltiazem, baby aspirin, furosemide, atorvastatin, and nitroglycerin (NTG) sublingual (S.L.) as needed, and his admitting diagnosis is heart failure.
Initial assessment
Mr. Barrett is pale, diaphoretic, and dyspneic. He says he feels week and has nonradiating chest pressure that he rates as 3 on the 0-to-10 assessment scale. On auscultation, you hear coarse rales in the lower two-thirds of the lungs and scattered expiratory wheezes. You note positive jugular venous distension and an S3 heart sound. Mr. Barrett’s vital signs are heart rate 104 beats/minute, respiratory rate 34 breaths/minute, BP 176/98 mmHg, and oxygen saturation 85% on 2 L/minute by nasal cannula. His ECG shows sinus tachycardia with frequent premature ventricular contractions. You place Mr. Barrett in high Fowler’s position, and call the rapid response team (RRT).
On the scene
The RRT arrives and orders a 100% nonrebreather mask, arterial blood gases (ABG), a 12-lead ECG, chest X-ray, and a serum brain natriuretic peptide (BNP) level. Per RRT orders, you administer NTG 0.4 mg S.L. and furosemide 80 mg I.V. push, followed by a furosemide infusion at 5 mg per hour. Based on the preload reduction effects of these medications, you monitor Mr. Barrett’s BP and urinary output.
The ECG shows sinus tachycardia with no ST segment elevation, but with premature ventricular contractions and a left bundle branch block. The BNP level is 1,925 pg/mL, and ABG results are pH 7.48, partial pressure of carbon dioxide 31 mmHg, partial pressure of oxygen 67 mmHg, bicarbonate 26 mEq/L, and oxygen saturation 80%. The chest X-ray shows cardiomegaly with pulmonary vascular congestion and patchy infiltrates. Mr. Barrett’s primary care provider (PCP) orders a transfer to the ICU.
In the ICU
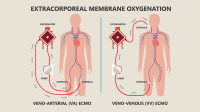
Mr. Barrett is started on a dobutamine infusion at 5 mcg/ kg/minute for positive inotropic support. Noninvasive ventilation with continuous positive airway pressure (CPAP) with 100% oxygen is applied to improve gas exchange and re-expand alveolar collapse. CPAP can decrease ventricular filling, which decreases preload and may cause hypotension, so the nurse monitors ABGs, oxygen saturation, BP, and heart rate.
The intensivist orders a transesophageal echocardiogram, which demonstrates left ventricular hypertrophy, anterolateral and inferior wall motion abnormalities, and an ejection fraction of 35%. Based on these results, the PCP orders enalapril 5 mg orally twice a day with parameters to hold medication if systolic BP is < 100 mmHg. Cardiac catheterization reveals less than 50% obstruction of the left anterior descending artery. Once he’s stable, Mr. Barrett is transferred back to your unit and cardiac rehabilitation is ordered.
Education
Acute cardiogenic pulmonary edema occurs with reduced cardiac muscle efficiency. This decrease in pump function results in increased pulmonary venous and capillary hydrostatic pressure, which allows fluid to accumulate in the lung interstitium, leading to hypoxemia. Impaired gas exchange can lead to acute type 1 respiratory failure.
Discharge instructions for Mr. Barret include take all medications as prescribed, contact his PCP if he experiences changes in his signs and symptoms, monitor daily weights, maintain low sodium intake, and stay active based on PCP recommendations.
*Names are fictitious.
Lisa Huffman is an assistant college lecturer at Cleveland State University in Cleveland, Ohio.
Selected references
Purvey M, Allen G. Managing acute pulmonary edema. Aust Prescr. 2017;40(2):59-63.
Sovari AA. Cardiogenic pulmonary edema treatment & management. Medscape. December 21, 2017. emedicine.medscape.com/article/157452-treatment
ant6-Rapid Response-513