An estimated 25,500 Americans died from falls in healthcare and community settings in 2013. Countless more suffered life-changing injuries, such as fractures, internal injuries, and traumatic brain injury. Experts estimate that more than 84% of adverse events in hospital patients are related to falls, which can prolong or complicate recovery. This article identifies risk factors for falls, explains how falls are classified, and describes how to perform a fall-risk assessment.
To monitor falls incidence in a consistent manner, healthcare professionals need to agree on the definition of a fall. A widely accepted definition is “an unplanned descent to the floor with or without injury to the patient.” The nursing diagnosis for risk of falls is “increased susceptibility to falling that may cause physical harm.”
To help identify patients’ risk factors for falls and guide interventions to prevent falls in acute-care settings, falls commonly are classified as anticipated physiologic falls, unanticipated physiologic falls, or accidental falls.
In addition, some clinicians classify risk factors as intrinsic or extrinsic. Intrinsic risk factors for falls—those originating within the individual—include:
- low blood pressure or orthostatic hypotension caused by standing, dehydration, or muscle weakness (most notable in the lower extremities)
- impaired mobility, unstable gait, and poor balance due to pain, musculoskeletal deformities, or neurologic disorders
- limited physical-activity endurance
- foot problems that cause pain or paresthesias (such as peripheral neuropathy)
- impaired vision due to poor depth perception, glaucoma, or cataracts.
Extrinsic risk factors originate outside the individual. They include conditions in the physical environment, such as poor lighting, clutter, a slippery floor due to a spill, and an uneven threshold.
Risk factors for anticipated physiologic falls
Risk factors for anticipated physiologic falls include an unstable or abnormal gait, a history of falling, frequent toileting needs, altered mental status, and certain medications. Among hospitalized older adults, about 38% to 78% of falls can be anticipated. Evidence shows that one-third of reportable falls with injuries in hospitalized older adults are linked to bathroom use; more than half are associated with medications known to contribute to falls, such as antianxiety and antipsychotic drugs. Also, about 40% of falls occur within 30 minutes of an hourly rounding visit by healthcare providers.
Assess the patient for diseases and disorders that affect the cardiovascular, respiratory, neurologic, or musculoskeletal system. Also consider possible effects of treatment for these diseases; many medications increase the fall risk by causing dizziness, drowsiness, or confusion. Perform a thorough medication reconciliation to identify potential high-risk drugs, including over-the-counter products (such as diphenhydramine, commonly used for allergic rhinitis or as a sleep aid). As a rule of thumb, the more medications a patient uses, the higher the fall risk due to adverse drug effects and drug-drug or drug-disease interactions. Also, make sure you’re familiar with the American Geriatric Society Beers Criteria for potentially inappropriate medication use in older adults.
Risk factors for unanticipated physiologic falls
Risk factors for unanticipated physiologic falls include conditions such as seizures, syncopal episodes, and delirium. These falls may occur with a temporary change in physical or cognitive function and unfamiliar surroundings. Such falls may be unanticipated if the patient is otherwise at low risk for falls.
Direct nursing interventions toward post-fall care and preventing injury in case of another fall. Currently, no tool exists to guide nurses and other healthcare team members in assessing risk for injury from unanticipated falls. Persons ages 85 or older, those with osteoporosis, and those taking anticoagulants are at greatest risk of injury from these falls.
Risk factors for accidental falls
Accidental falls can stem from slipping, tripping, or other accidents. They’re frequently linked to extrinsic factors. To help reduce risk, evaluate the physical environment continually for safety hazards. Be aware that falls in hospitals and other acute-care settings most often occur in patient rooms, when patients are alone, or when they attempt to go to the bathroom. Many hospitals are reevaluating the design of patient rooms and bathrooms to decrease environment-related falls. A redesign that enables nurses to document at the bedside rather than at a remote station provides increased patient-safety surveillance and decreases the potential for falls.
Be sure to consider assistive devices when evaluating extrinsic risk factors that can cause accidental falls. Canes, walkers, and wheelchairs are meant to increase the patient’s support and improve balance and mobility. But many patients aren’t properly taught how to use them; in some cases, the device is damaged or the wrong size for the patient. In long-term care facilities, the highest incidence of falls occurs during transfers—when the patient moves from wheelchair to bed or gets up from an unbraked wheelchair. Physical therapists can help evaluate assistive devices and determine if they are the right size and are being used properly; they also can provide education on their use.
Also consider other extrinsic risk factors for accidental falls. For instance, check the patient’s footwear and clothing, which can affect mobility. Are the patient’s pants too long?
Fall-risk screening and assessment
Screening and assessment can help nurses and other healthcare professionals identify patients at risk for falls. Fall-risk screening determines if the patient is at risk for falls and indicates whether a more in-depth multifactorial assessment should be done. Fall-risk assessment provides a systematic way to check for valid and reliable causes of falls in a particular patient and identify factors for which interventions are known to reduce the fall risk.
Screening
When screening patients for fall risk, check for:
- history of falling within the past year
- orthostatic hypotension
- impaired mobility or gait
- altered mental status
- incontinence
- medications associated with falls, such as sedative-hypnotics and blood pressure drugs
- use of assistive devices.
Also, be aware that patients tethered to I.V. lines or other equipment are at increased risk for falls.
Assessment
In long-term and acute-care settings, fall-risk assessment is required for all patients on admission, transfer to a new unit, after a change in the level of care or the patient’s condition, and after a fall. Because falls have multifactorial causes, an interprofessional team should collaborate in the comprehensive assessment. A standard assessment combines a systematic assessment with clinical decision making, targeted interventions, care planning, and communication with other healthcare professionals.
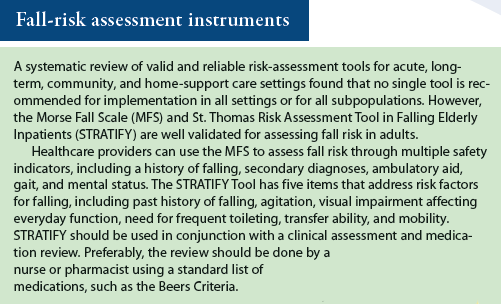
Nearly 50 fall-risk assessment instruments exist. Typically, these tools use a scoring system that measures the cumulative effect of known risk factors. (See Fall-risk assessment instruments.) When selecting an assessment tool, focus on identifying key risk factors that can guide interventions to reduce or mitigate fall risk.
Some tools use a scoring system with cut-off values for patients at high risk. But even if the patient has a low score, don’t let this distract you from implementing interventions to reduce the risk of falling if the patient has identifiable and preventable risks. Also, be aware that if all or many patients are placed in a high-risk category, staff may be less likely to individualize care plans when particular risks are identified for a particular patient.
Information from the assessment guides diagnosis and implementation of a consistent plan of care. A critical step in this multifaceted process is communicating the patient’s fall risk and required interventions to colleagues, the patient and family, and significant others who need to support the interventions. Using a systematic process to identify and address the fall risk can nearly eliminate anticipated falls, prevent unanticipated falls from recurring, and significantly decrease accidental falls.
Beverly Lunsford is an assistant professor in the School of Nursing at George Washington University (GW) in Washington, DC; director of GW’s Center for Aging, Health and Humanities; and director of the Washington D.C. Area Geriatric Education Center Consortium. Laurie Dodge Wilson is an assistant clinical professor at GW School of Nursing.
Selected references
Agency for Healthcare Research and Quality. Preventing falls in hospitals: a toolkit for improving quality of care. January 2013. www.ahrq.gov/professionals/systems/hospital/fallpxtoolkit/fallpxtk5.html
American Geriatrics Society, British Geriatrics Society. AGS/BGS clinical practice guideline: prevention of falls in older persons. New York, NY: American Geriatrics Society; 2010.
American Geriatric Society. 2012 AGS Beers criteria for potentially inappropriate medication use in older adults. http://www.americangeriatrics.org/files/documents/beers/2012AGSBeersCriteriaCitations.pdf
Boushon B, Nielsen G, Quigley P, et al. How-to guide: reducing patient injuries from falls. Cambridge, MA: Institute for Healthcare Improvement; 2012. http://www.ihi.org/resources/Pages/Tools/TCABHowToGuideReducingPatientInjuriesfromFalls.aspx
Centers for Disease Control and Prevention. STEADI (Stopping Elderly Accidents, Deaths and Injuries). Make STEADI part of your medical practice. Last updated May 12, 2015. www.cdc.gov/homeandrecreationalsafety/Falls/steadi/index.html
Stevens JA, Phelan EA. Development of STEADI: a fall prevention resource for health care providers. Health Promot Pract. 2013; 14(5):706-14.
Willy B, Osterberg CM. Strategies for reducing falls in long-term care. Ann Longterm Care. 2014; 2(1). www.annalsoflongtermcare.com/article/strategies-for-reducing-falls-long-term-care



















2 Comments.
Hi,
Thank you for sharing this wonderful topic and It’s perfectly fine if you decide not to include SafetyCulture on the list, but is it possible for me to get some feedback? It will help me reach out to you with more relevant information in the future :D.
Thank you for your time. Keep up with awesome content!
id there any study regarding the clinical judgement of nurses as criteria for assessment of fall risk, if so, what about its otcome?