The power of RNs to effect change
By Sametria McCammon, MSPH, and Sharon Morgan, MSN, RN, NP-C
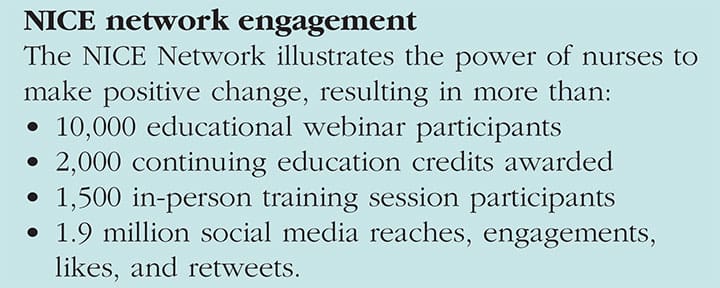
For 2 years, the Nursing Infection Control Education (NICE) Network, a partnership between the American Nurses Association (ANA), the Centers for Disease Control and Prevention (CDC), and 20 nurse specialty organizations, has empowered nurses to protect themselves and their patients by developing and disseminating customized infection prevention and control (IPC) training opportunities. Although established to reengage nurses in basic IPC protocols to prepare for the next emerging disease threat, the Network also reaches students, faculty, and other healthcare professionals. (See NICE network engagement.)
Our strategy
The Network achieved its goal by first gathering data on current nursing curricula in IPC and opportunities to improve nurses’ adherence to IPC protocols in nursing practice. It used these findings to develop webinars, in-person training sessions, and targeted communications and fact sheets. The Network focused its evaluation on the impact of nurses’ participation in its in-person training sessions at member conferences.
What we learned in the assessment
The following competencies are identified opportunities to enhance nursing student IPC knowledge:
- Articulate a systematic approach to record surveillance data (for example, infection rates on nursing units, central line–associated bloodstream infections, and catheter-associated urinary tract infections).
- Understand specific rates and ratios (for example, provider-specific, unit-specific, device-specific, procedure-specific, standardized infection ratio).
- Reinforce cleansing principles of the care environment and using appropriate disinfecting agents.
Furthermore, the assessment showed that nurses recognize the significance of hand hygiene, patient involvement in the IPC process, and patient advocacy to reducing healthcare-associated infections.
But many nurses reported lack of time and too many patients as barriers to adhering to known protocols. Therefore, the Network’s IPC educational training opportunities focused on:
- providing real-time, evidence-based education that establishes the “why” behind the actions
- explaining the relationship between the nurse’s actions and the patient’s outcomes
- sharing with nurses and organizations resources related to data collection, monitoring and surveillance programs, and developing a formal mechanism for accountability.
 Impact of in-person training sessions
Impact of in-person training sessions
In a self-reported, 3-month follow-up survey of changes in practice based on information learned during a NICE Network training session, 17.2% of nurses changed infection control practice, 13.6% changed student and colleague education, and 11.1% changed their interaction with peers and other healthcare providers. For the nurses who haven’t made changes yet, 20% reported lack of time and 18% said that they plan to make changes.
Next steps
The Network will continue to collaborate and share IPC information with the nursing community. All resources—specifically, PDFs of in-person training session materials and on-demand webinars with continuing education credits produced through the Networkwill be available on ANA’s website. The NICE Network has shown how nurses can lead change and continue to be empowered to maintain safety for all.
Sametria McCammon and Sharon Morgan are senior policy advisors in Nursing Practice and Work Environment at ANA.
ant7-ANA NPWE-618


















