Learn about central line care and maintenance.
Takeaways:
- Advocate for newer central line dressing options (such as subcutaneous securement) that avoid suturing.
- The Centers for Disease Control and Prevention update to the 2011 guidelines for preventing intravascular catheter-related infections made using a chlorhexidine-impregnated dressing a Category 1A recommendation (the strongest recommendation).
- When a central line–associated bloodstream infection occurs, uncovering the cause and developing an action plan are key to preventing future infections.
Editor’s note: This is the second article in a two-part series on central line–associated bloodstream infections (CLABSI). Part one focused on CLABSI indications and insertion (myamericannurse.com/revisiting-clabsi-prevention-strategies-part-1).
WHEN a patient’s healthcare team determines that a central line is needed (see myamericannurse.com/revisiting-clabsi-prevention-strategies-part-1), proper maintenance is required to prevent CLABSI and prompt action is needed if one occurs.
Central line care and maintenance
Before applying a dressing to a central line insertion site, secure the device. Advocate for newer options (such as subcutaneous securement) that avoid suturing, allowing the line to be more easily cared for.
When choosing a dressing, consider that in 2017, the Centers for Disease Control and Prevention (CDC) made one update to the 2011 guidelines for the prevention of intravascular catheter-related infections: Using a chlorhexidine-impregnated dressing is now a Category 1A recommendation (the strongest recommendation) for nontunneled, short-term catheters. The CDC specifies that this type of dressing should carry a U.S. Food and Drug Administration (FDA)–cleared label with an indication to prevent infections.
strongest recommendation) for nontunneled, short-term catheters. The CDC specifies that this type of dressing should carry a U.S. Food and Drug Administration (FDA)–cleared label with an indication to prevent infections.
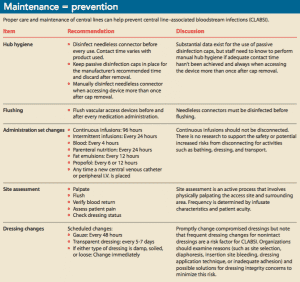
Once the dressing is in place, follow the basics of central line care and maintenance, including hand hygiene (before and after contact with the patient or the patient’s environment and whenever moving from dirty to clean tasks), hub hygiene, device flushing, appropriate administration set change practices (continuous versus intermittent and infusate specific requirements), site assessment, and maintaining a clean, dry, and intact dressing. (See Maintenance = prevention.)
Central line necessity
Central line care also should include daily review of its necessity. Use the electronic health record (EHR), with specific criteria to be verified as part of the daily assessment. Best practice alerts for all staff will remind providers to carefully review the patient’s current and anticipated vascular access needs and prompt a purposeful decision to keep or discontinue the line. Auditing (through chart review and direct observation) provides an opportunity to address correctable process failures before they result in patient harm. These audits can help aggregate data on device use and adherence with other prevention strategies. The combination of approaches offers a more robust understanding than relying only on retrospective review. The decision to discontinue or de-escalate a central line should be made via interprofessional rounds, with input from pharmacy and vascular access specialists, and it should include an evaluation of the patient’s postdischarge needs.
What to do when a CLABSI occurs
If a CLABSI is suspected, the provider will order blood cultures. (See Specimen collection: Best practices.) Any diagnosed CLABSIs should be treated as life-threatening, and antibiotics specific to the organism should be initiated. Infection preventionists, vascular access specialists, providers involved with device insertion, and frontline staff should review the case in detail, looking for potential contributing factors.
Specimen collection: Best practicesSpecimen collection practices influence the likelihood of a culture providing the most accurate clinical information to identify a central line–associated bloodstream infection (CLABSI). CLABSIs are identified by a positive blood culture (with a recognized pathogen) in a patient with a central venous catheter (in place for at least 3 calendar days) in the absence of another defined infection (following Centers for Disease Control and Prevention site-specific requirements). This is different from the clinical definition of catheter-related bloodstream infections, which also relies on additional testing (including methods such as paired cultures, time to positivity analysis, or culturing the tip of the catheter if it has been removed). These best practices will help ensure correct specimen collection:
|
Open discussion
Uncovering the cause of the CLABSI and developing an action plan are key steps to preventing future infections. One method of review is apparent cause analysis. (At Methodist Hospitals, the analysis is facilitated by a member of the infection prevention team who’s a clinical nurse specialist with expertise in critical care and is certified in infection control and vascular access.)
Start with an initial EHR chart review to provide patient and situation background information. Within a week of identifying the infection, the clinical staff from the units who provided care should gather to review all aspects of the case—from line insertion to any care difficulties (dressing problems, daily bathing documentation, tubing changes, and needleless connector change documentation)—and identify improvement opportunities. They then can create an action plan with measurable goals. (See Questions lead to answers.)
When conducted in a collaborative, nonpunitive manner, this discussion is a powerful tool for understanding prevention opportunities. Infection preventionists must rely on information in the EHR to determine whether the patient has developed a CLABSI, but performance improvement requires open discussion with staff and direct observations of care.
Questions lead to answersAsking the right questions can help prevent central line–associated bloodstream infections. For example, to determine if proper techniques are being used to avoid infection from Staphylococcus aureus, a skin pathogen, observe staff and ask:
|
Information sharing
Share review and discussion findings through learning opportunities for all staff. Acknowledge different learning styles and ask for team input about the best way to distribute the information.
When you help staff understand what contributed to CLASBI, they can focus on preventing infections rather than responding to them. In addition to the complete case review, share information about specific organisms and microbiology related to skin, environment, water, and infusates. This knowledge can help tailor discussions to gather more information in the areas most strongly associated with the specific cause.
Causative organisms. Staphylococcus aureus is frequently encountered on the skin, and gram-negative organisms also cause significant disease in patients with central lines. A recent study identified that the source of Escherichia coli bloodstream infections was rarely the vascular catheter, but frequently associated with a urinary or GI source or febrile neutropenia. In the absence of a defined secondary infection at those or other body sites, these infections are identified as a CLABSI using current, mandated surveillance definitions with the exception of those in a severely neutropenic patient.
Candidemia. Candidemia should raise specific questions for review. Parenteral nutrition provides a substrate for this organism to thrive and has been implicated in outbreaks. Carefully review the consistency of 24-hour interval administration set and needleless connector changes for this infusate. Standards also support a dedicated lumen for parenteral nutrition as well. Some species, such as Candida parapsilosis, are associated with failure to comply with basic infection prevention practices.
Environmental contamination. Direct staff to look at environmental issues, including cleaning frequently touched surfaces (such as bedrails), patient hand hygiene (particularly with incontinence), and general hygiene and bathing practices. Also consider the possibility of hub or vascular access site contamination if dressings are compromised.
These are just a few examples of how knowledge of specific organisms can lead to more fruitful conversations. Talk with pharmacists, microbiologists, infection preventionists, and the hospital epidemiologist if you have questions about how to include these discussions in your review process.
The right care
Personal accountability for care includes receiving feedback when expectations aren’t met. Unit score cards are common, but taking these issues directly to individual nurses can help make them personal. Engage bedside staff in chart audits and vascular access rounds to help bolster awareness. For staff who are interested in furthering their knowledge and demonstrating their role in vascular access, board certification (vacert.org) is an option. This credential is for teams placing lines and for anyone with a role in vascular access, including frontline staff and infection prevention teams.
Staff involvement in reviewing CLABSI cases and the policies and process measures that help prevent infections can help focus the team on ensuring that the right care is provided for every patient, every line, every single time.
Michelle DeVries is senior infection control officer for Methodist Hospitals in Gary, Indiana, and is an adjunct research fellow at Griffith University in Australia. She serves on the speakers’ bureau for Access Scientific, Becton Dickinson, Ethicon, and Eloquest.
Selected references
Centers for Disease Control and Prevention. Bloodstream infection event (central line-associated bloodstream infection and non-central line associated bloodstream infection). January 2019. cdc.gov/nhsn/pdfs/pscmanual/4psc_clabscurrent.pdf
Centers for Disease Control and Prevention. 2017 Updated recommendations on the use of chlorhexidine-impregnated dressings for prevention of intravascular catheter-related infections. July 17, 2017. https://www.cdc.gov/infectioncontrol/pdf/guidelines/c-i-dressings-H.pdf
Egan GM, Siskin GP, Weinmann R 4th, Galloway MM. A prospective postmarket study to evaluate the safety and efficacy of a new peripherally inserted central catheter stabilization system. J Infus Nurs. 2013; 36(3):181-8.
Garcia RA, Spitzer ED, Kranz B, Barnes S. A national survey of interventions and practices in the prevention of blood culture contamination and associated adverse health care events. Am J Infect Control. 2018;46(5):571-6.
Guducuoglu H, Gultepe B, Otlu B, et al. Candida albicans outbreak associated with total parenteral nutrition in the neonatal unit. Indian J Med Microbiol. 2016;34(2):202-7.
Huang SS, Septimus E, Kleinman K, et al. Targeted versus universal decolonization to prevent ICU infection. N Engl J Med. 2013;368 (24):2255-65.
Morrison T, Raffaele J, Brennaman L. Impact of personalized report cards on nurses managing central lines. Am J Infect Control. 2017;45 (1):24-8.
Pittiruti M, Scoppettuolo G, Dolcetti L, et al. Clinical experience of a subcutaneously anchored sutureless system for securing central venous catheters. Br J Nurs. 2019;28(2):S4-14.
Pronovost P, Needham D, Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. 2006;355(26):2725-32. Erratum in: N Engl J Med. 2007;356(25):2660.
Septimus E, Hickok J, Moody J, et al. Closing the translation gap: Toolkit-based implementation of universal decolonization in adult intensive care units reduces central line-associated bloodstream infections in 95 community hospitals. Clin Infect Dis. 2016;63(2):172-7.
Timsit JF, Bouadma L, Ruckly S, et al. Dressing disruption is a major risk factor for catheter-related infections. Crit Care Med. 2012;40(6): 1707-14.
Xiong Z, Chen H. Interventions to reduce unnecessary central venous catheter use to prevent central-line–associated bloodstream infections in adults: A systematic review. Infect Control Hosp Epidemiol. 2018; 39(12):1442-8.
Ziegler MJ, Pellegrini DC, Safdar N. Attributable mortality of central line associated bloodstream infection: Systematic review and metaanalysis. Infection. 2015;43(1):29-36.