When looking back on nursing school, most nurses probably remember diagnosing themselves with the “disease of the day.” Nursing students question every symptom and ailment they have ever experienced as they dive into the details of unfamiliar diseases. You may have even thought you had von Willebrand disease (VWD) when you first learned of it.
Whether or not you suspected you had VWD, you probably don’t remember much about it and you might not have cared for anyone with the disease, since experts estimate that only about 1% of the population has the condition. But VWD is the most common inherited bleeding disorder, which means it’s important for you to understand the basics of the disorder so you can deliver the care patients with VWD need.
Overview
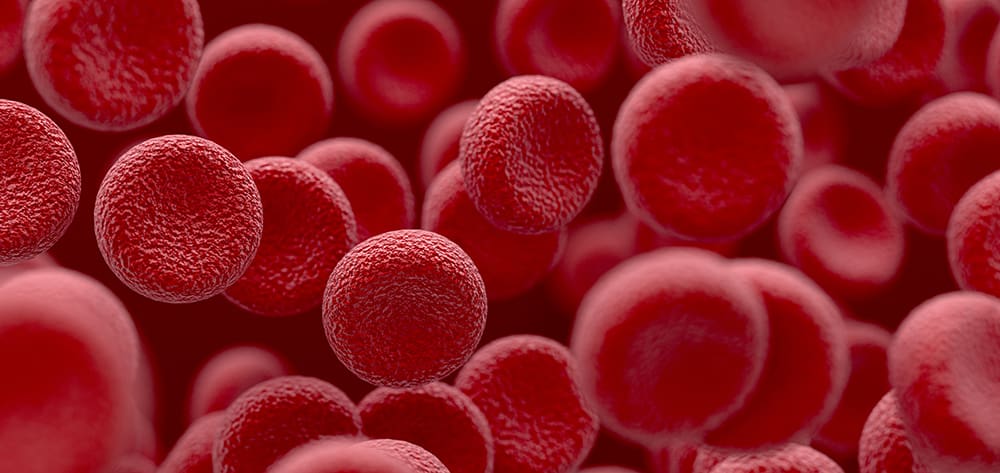
Dr. Erik von Willebrand first described VWD in 1926. This congenital bleeding disorder is characterized by low or ineffective von Willebrand factor, which is essential for platelet adhesion and helps to transport factor VIII in the blood. VWD causes a variety of bleeding symptoms such as abnormal bruising, heavy menstrual periods, nosebleeds that are difficult to stop, mucosal bleeding, and abnormal bleeding after surgery or trauma. While VWD is not curable, it is treatable.
VWD can be inherited from either parent. Although it affects both men and women, women are diagnosed more frequently, most likely because of symptoms related to heavy menstrual periods. (See Types of VWD below.)
Types of VWDVWD occurs in three major types. Type 1, the most common, is characterized by low levels of von Willebrand factor. People with type 1 VWD also may have low levels of factor VIII. Type 1 causes mild symptoms. People with type 2 VWD have a normal amount of VWF, but the factor doesn’t function properly. Type 2 VWD is broken down into subtypes 2A, 2B, 2M, and 2N. The defective clotting process differs in each subtype, and each is caused by a different genetic mutation. Treatment depends on the subtype, so proper diagnosis is essential. People with type 2 VWD can experience mild to moderate bleeding problems. Type 3 VWD is rare and usually only occurs in people who have two parents with VWD. This type results in little or no von Willebrand factor and low levels of factor VIII. Type 3 VWD is severe and requires a more aggressive treatment plan. These patients must be diligent in being aware of bleeding symptoms and get immediate treatment when bleeding occurs. |
Diagnosis
There is no single test for VWD, which can make diagnosis challenging. The first step in evaluating a patient is to obtain a complete family history. Be aware that because of mild unnoticed symptoms, a family history of VWD or abnormal bleeding may not always be present.
Next, initial laboratory tests are done to eliminate other causes of abnormal bleeding. These tests include a complete blood count, activated partial thromboplastin time (aPTT), prothrombin time (PT), fibrinogen level, and platelet count.
If these tests fail to identify a cause for bleeding, additional testing is done. The tests more specific to VWD are von Willebrand factor antigen (VWF:Ag), von Willebrand factor ristocetin cofactor (VWF:RCo), and a factor VIII level. The VWF antigen test will show the amount of VWF in the blood. A level less than 30 IU/dl is definitive for VWD; however, a level between 30 IU/dl and 50 IU/dl also can be indicative. The VWF:RCo test indicates the functionality of VWF; that is, how well it is working.
A hematologist familiar with VWD must evaluate the patient’s history and the results of all of these tests. Further testing may be required. For example, if VWD is confirmed, a multimeric test is done to determine which type of VWD is present. If a patient has a bleeding history and the VWD testing is negative, a platelet aggregation may be completed to explore a different diagnosis. Also, testing multiple times is recommended because of events that may alter levels temporarily such as medications, pregnancy, menstrual cycle, breastfeeding, recent surgery, or stress.
Another important aspect of diagnostic testing is specimen handling. Results may be inaccurate if the blood sample is not processed in a timely manner. A sample collected in an office and delivered to the lab at the end of the day will not be accurate. Consulting with a bleeding disorder center or a hematologist with experience in diagnosing and treating bleeding disorders will ensure proper evaluation and diagnosis.
Considerations for women
As noted earlier, VWD is most often diagnosed in women. Because most boys with VWD typically only experience abnormal bleeding with severe injury or surgery, they may never be diagnosed. The bruising and nosebleeds that sometimes occur with VWD may be overlooked in young boys.
When VWD is diagnosed in a young girl, it’s often after generations of women have experienced heavy menstrual cycles. For many years, mothers explain to their daughters that heavy periods are just normal for their family. When a diagnosis is finally made, the family realizes that VWD has probably been in the family for a long time. Sometimes multiple generations of women will have early, unnecessary hysterectomies to relieve the symptoms.
Girls with VWD often experience heavy bleeding during their first period. In fact, one study indicated that this was the most common first bleeding symptom in type 1 VWD. Girls should be evaluated by a gynecologist early to carefully document menstrual cycles and recognize irregular or abnormal bleeding.
Girls with VWD live a normal life once bleeding is controlled with proper treatment, but continued collaboration between the hematologist and gynecologist is important throughout adolescence and young adulthood.
VWD and pregnancyWhen a woman with VWD decides to have a baby, she must consider her bleeding disorder. Typically, levels of VWF and factor VIII increase to normal during pregnancy. Testing is required throughout the pregnancy to determine bleeding risk. Miscarriages related to bleeding disorders are not common, unlike miscarriages related to clotting, which are very common. Bleeding problems also do not occur frequently during delivery. The primary concern is bleeding during the postpartum period, after the VWF and factor VIII levels have decreased. Up to 30% of women with VWD experience postpartum hemorrhage. Precautions should be taken during delivery to avoid complications. Risk of hemorrhage can be decreased by avoiding procedures such as episiotomies and avoiding the use of forceps, vacuums, and fetal scalp electrodes. While women with mild or moderate VWD can deliver vaginally without difficulty, those with severe type 3 VWD may require a Cesarean section if the second stage of labor is prolonged. Patients should meet with the anesthesiologist before delivery to discuss options for pain control. VWD does not eliminate the choice of an epidural; however, the anesthesiologist must be included in the plan of care and collaborate with the hematologist and obstetrician to provide the safest treatment. |
Treatment
Treatment depends on the type of VWD and should be decided by a hematologist. Options include the following:
- Hormonal treatments such as oral contraceptives and some intrauterine devices are highly effective in controlling menorrhagia. In fact, 88% of women with VWD report improvement in bleeding symptoms when treated only with oral contraceptives.
- Desmopressin (DDAVP) is effective in most patients with type 1 VWD and some patients with type 2. Recovery testing must be done to determine its effectiveness. During a recovery test, a blood sample is obtained before the medication is given and 30 to 60 minutes after administration. This test helps determine if the medication increases the patient’s factor levels enough to prevent or stop bleeding.
- Replacement factor made from plasma-derived concentrates can be used in any patient with VWD, but must be used in all patients with type 3 and in some patients with type 2. Replacement factor is also used when patients don’t respond to DDAVP.
- Antifibrinolytics such as aminocaproic acid and tranexamic acid are used in conjunction with factor or DDAVP to treat bleeding. Antifibrinolytics stabilize a clot by preventing it from breaking down too early, which would cause bleeding. Without antifibrinolytics, bleeding may occur several days or weeks after a procedure involving mucosal tissue. Antifibrinolytics are effective in treating mucosal bleeding such as with dental surgery, menstrual bleeding, nosebleeds, and gastrointestinal bleeding.
Patients with VWD should avoid medications that can increase bleeding risks, for example, aspirin and nonsteroidal antiinflammatory drugs (NSAIDS). Pain relievers such as acetaminophen are a better choice because they don’t increase the risk of bleeding.
A valuable resource
Most people with VWD live normal daily lives, but complications can arise with surgery or trauma. It’s important for caregivers in the hospital and other healthcare facilities to be familiar with VWD and the steps to take to ensure hemostasis and decrease the risk of complications related to the bleeding disorder. This is effectively done through education and collaboration with a hematologist.
Remember, sometimes knowing where to find information is as important as trying to remember everything you learn. A great resource for up-to-date information regarding bleeding disorders is a hemophilia treatment center. The network of centers is available for education, treatment information, and sometimes even insurance benefit assistance. Many centers have genetic counselors, social workers, and physical therapists in addition to nurses and hematologists. They are devoted to caring for patients with bleeding disorders and will be happy to help. You can find a list of hemophilia treatment centers at www.hemophilia.org.
Denise Hitch is nurse coordinator in the East Tennessee Comprehensive Hemophilia Center at the University of Tennessee Medical Center in Knoxville.
Selected references
The Diagnosis, Evaluation, and Management of von Willebrand Disease. U.S. Department of Health and Human Services National Institutes of Health. National Heart, Lung, and Blood Institute. December 2007. NIH publication No. 08-5832.
Von Willebrand Disease in Women. American College of Obstetricians and Gynecologists Committee Opinion. Number 451. December 2009.
Pacheco LD, Costantine MM, Saade GR, et al. von Willebrand disease and pregnancy: a practical approach for the diagnosis and treatment. Am J Obstet Gynecol. 2010;203(3):194-200.
National Heart, Lung, and Blood Institute. In brief: your guide to von Willebrand disease. http://www.nhlbi.nih.gov/health/public/blood/vwd_in_brief.htm Accessed May 10, 2013.